The Passing of Splenic Flexure
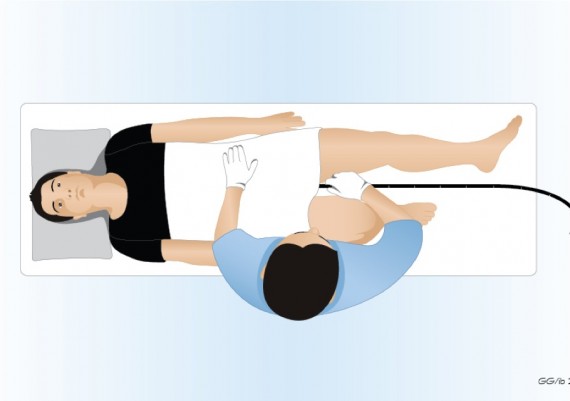
The passing of the splenic flexure is usually tackled with the patient in supine position (fig. 1) to favor the opening of the splenic angle.
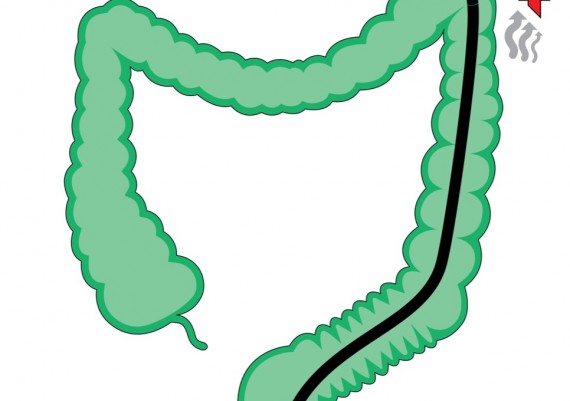
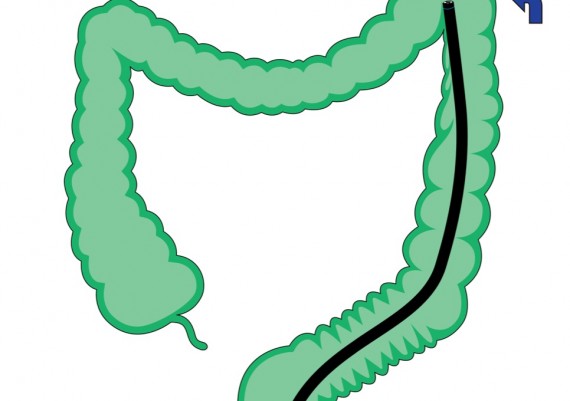
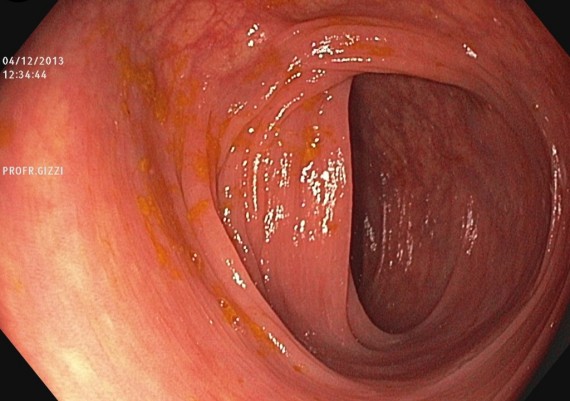
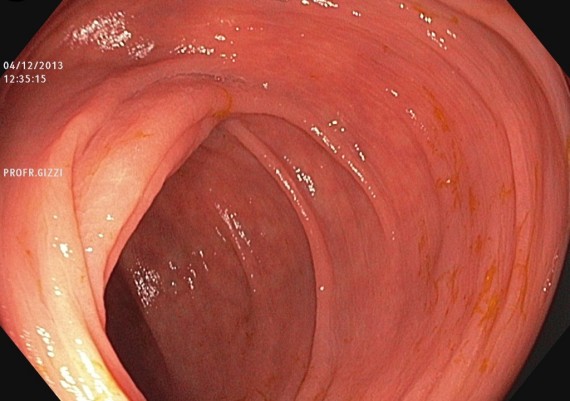
If the sigmoid has been correctly straightened, once the tip of the scope is next to the curve, the splenic flexure is passed aspirating air and deflecting the tip on the left, while the nurse assistant gradually pushes forward the shaft of the scope forward (fig. 2 A-B).
Fig. 2 A-B: if the endoscopist has properly straightened the sigmoid loops, after calibrated deflation (A), the tip of the scope is turned to the left (B), the splenic flexure is quite easily passed and the scope enters the distal portion of the transverse colon.
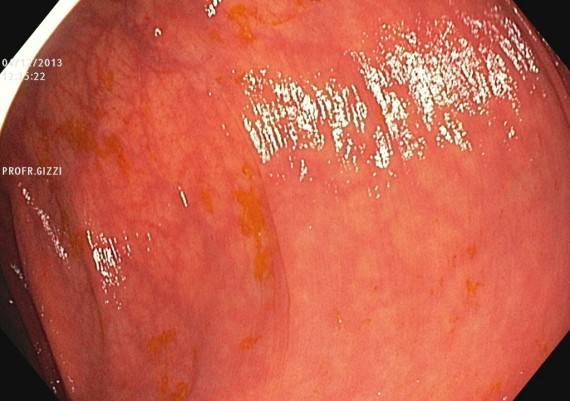
The achieved passing of the flexure is confirmed by the visualization of the triangular-shaped lumen which is characteristic of the transverse colon (Fig. 3).
Fig. 3: the triangular-shaped lumen of the transverse colon witnesses the passing of the splenic flexure.
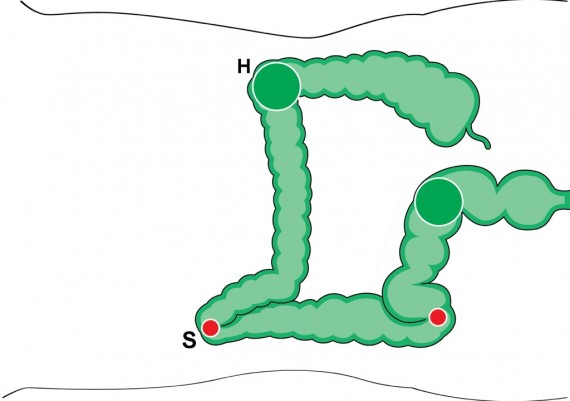
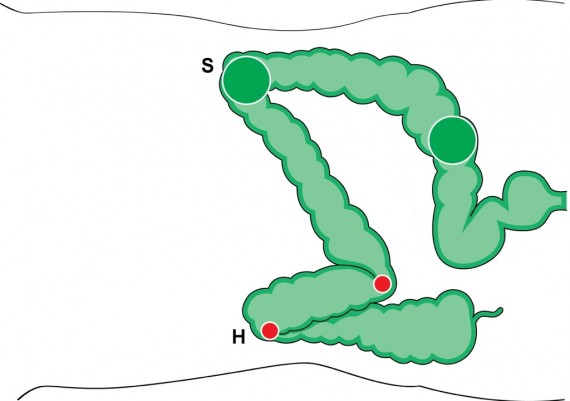
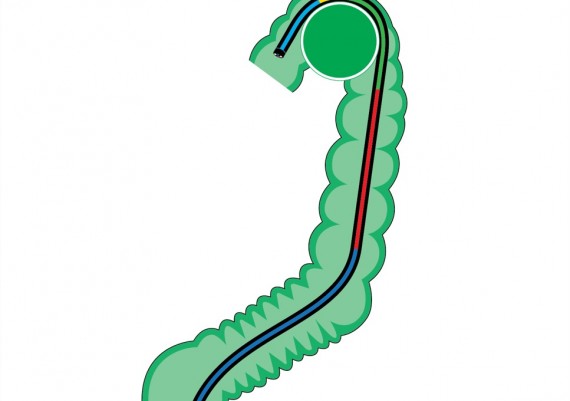
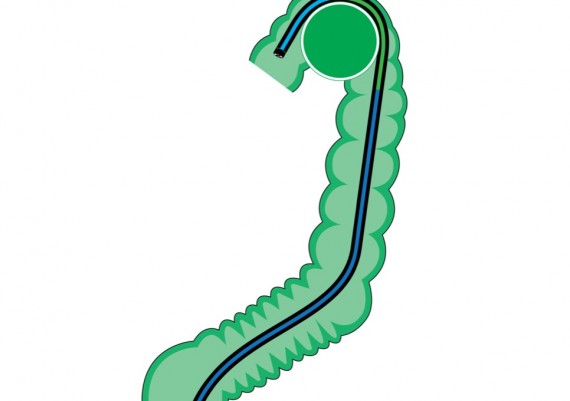
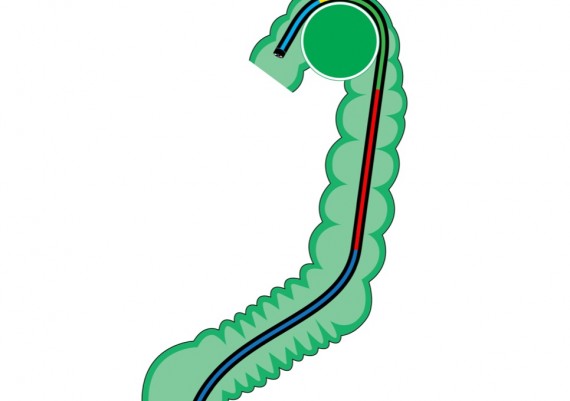
If the splenic flexure has a very acute angle, the push of the colonoscope by the nurse does not obtain the advancement, but rather a concentrated pressure (“walking stick handle”) that pushes high up the splenic flexure, causing pain to the patient. Any further insertion force favors the re-looping of the sigmoid colon, frustrating the efficacy of the maneuver (fig. 4 A-B).
Fig. 4 A-B: if the splenic flexure is particularly angled, the “walking-stick handle” effect occurs (A) because the vector force on the shaft of the colonoscope is concentrated on a small area of the colonic wall (red circle). Any further pushing force exerted by the nurse frustrates the progression because favors re-looping of the sigmoid (B).
Also in this case, as for the acute angulations of the sigmoid colon, the aim of the endoscopist is to achieve a widening of the contact surface between colonoscope and colonic wall, that is an opening of the angle between the axis of the descending and the transverse colon in orer to facilitate sliding and progression of the colonoscope.
Standard Colonoscope
If using a standard colonoscope, the most immediate option is to ask the patient for a deep inspiration, testing whether this simple maneuver eases the progression (Fig. 5).
Fig. 5: In some cases, the deep inspiration transmits a pressure on the top of the splenic flexure which facilitates the passing of the scope into the distal transverse colon.
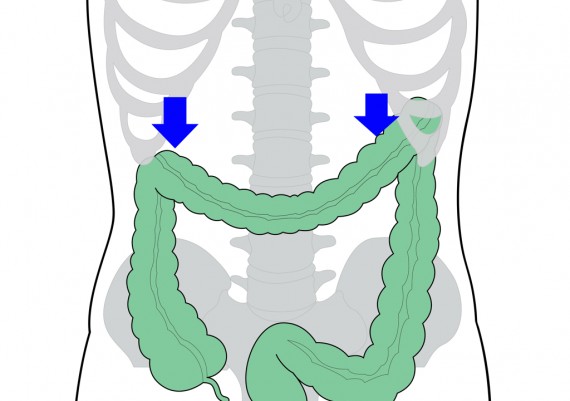
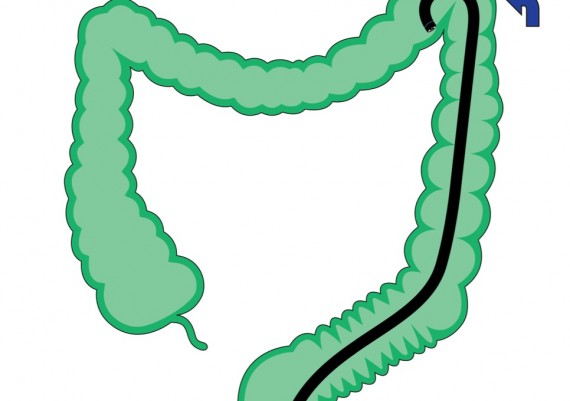
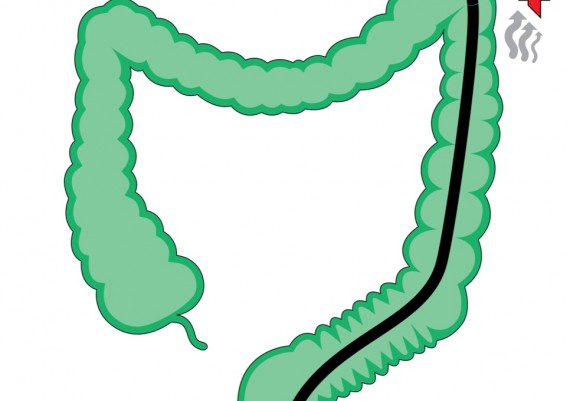
If the deep inspiration does not produces any favorable effect, the change of the patient’s position from supine to right lateral decubitus, in most cases facilitates the progression of the scope due to the modified opening of the splenic angle (fig. 6 A-D).
Fig. 6 A-D: the left lateral decubitus (A) favors the persistence of a “closed” angle (red circle - B) at the level of the splenic flexure (S), poorly modified by the supine position; with the patient in right lateral decubitus (C), the gravity favors the opening of the splenic angle (D – green circle) and the easy passing of the colonoscope.
Because of the gravity, this maneuver indices the sliding of the transverse colon toward the right abdominal quadrants, with traction on the distal segment of the transverse and subsequent widening of the angle between the axis of the descending colon and the axis of the transverse colon. In this position, after complete straightening of the scope, pushing can be resumed and progression occurs in most cases.
Variable Stiffness Colonoscope
In the impossibility to pass the splenic flexure, the colonoscope is straightened until the operator feels that the tip of the scope is free to move and that there is no resistance on the shaft. Then, the stiffness is increased to the maximum level (level 3), and the colonoscope is again pushed avoiding an excess tip deflection that would inevitably lead again to a walking-stick handle effect. The rationale behind the use of the variable stiffness function lies in the higher resistance of the scope to the passive flexion in the sigmoid colon, and therefore the ability to better transmit the vector force to the tip of the instrument (Fig. 7).
Fig. 7 A-D: the changes of the position of the patient modify the width of the angles between the fixed segments of the colon (descending and ascending) and the mobile ones (sigmoid and transverse). The gravity drags the mobile segments and transforms the acute angles (red circle) into obtuse angles (green circle), easier to intubate. Also the angle between the sigmoid and the descending colon is modified (S = splenic flexure; H = hepatic flexure).
Also in this case the passing of the splenic flexure can be facilitated by asking the patient for a deep inspiration that lowers the diaphragm and the flexure accordingly. Obviously, the change of patient’s position to the right side facilitates the progression into the transverse colon in difficult cases also with the variable stiffness colonoscope.
Passive bending colonoscope
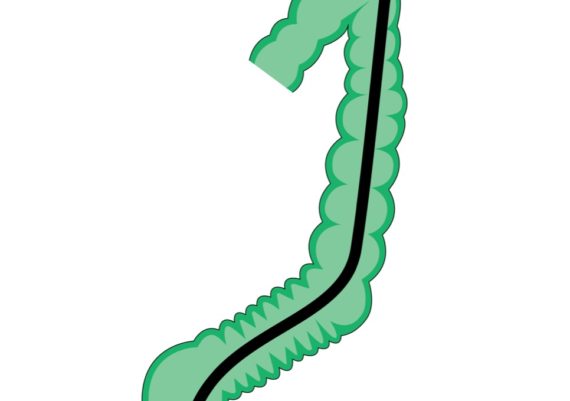
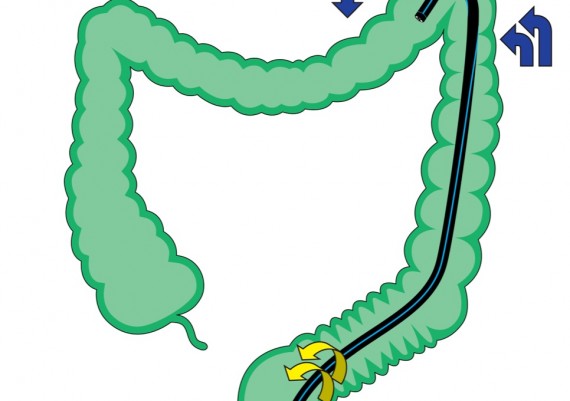
Beside a very looped sigmoid colon, the “passive bending” colonoscope is useful also in passing the splenic flexure. The basic mechanism follows what has already been described for other colonic segments, that is the widening of the contact arch between the colonoscope and the colonic wall (fig. 8 A-B).
Fig. 8: the ‘passive bending’ segment (yellow) bends passively when the distal tip of the scope exerts a consistent pressure on the colonic wall, widening the arched segment of contact between the scope and the colonic angle. The wider angle (green circle) obtained reduces the friction and the pressure, favoring the sliding and advancement of the colonoscope (A).
The ‘passive bending’ colonoscope also has a higher stiffness of the shaft. However, in cases of a particularly difficult splenic flexure, it is suitable to resort to ancillary maneuvers previously described (B).
Active Bending Procedure
The expert endoscopist performs the intubation of a very angled splenic flexure hooking the fold of the splenic angle to drag forward the non-bending segment of the colonoscope located next to the bending segment. With the patient in supine position, the first step is the complete aspiration of all the excess air (fig. 9 ).
Then the endoscopist starts to progressively turn the tip of the scope to the left (fig. 10)
When the lumen beyond the fold becomes visible, the endoscopist completes the left angulation of the tip and adds a downward tip deflection, rotating progressively the scope to the left (fig. 11)
Fig. 11: increasing the left angulation, the endoscopist bends the tip of the scope downward and rotates the scope to the left.
If following these combined maneuvers the lumen of the distal transverse colon becomes visible, the tipi s fully angled to hook the proximal edge of the splenic fold and drag the scope forward (fig. 12)
Fig. 12: if the endoscopist sees the lumen of the transverse colon, he/she can complete the full angulation of the tip to hook the splenic fold and drag the colonoscope forward.
The tip is now released and the pushing force allows to enter the distal transverse colon (Fig. 13).
Fig. 13: when the scope is sufficiently inserted in the transverse colon, the tip is released and the pushing force makes it pass the distal transverse colon.
Endoscopic Sequence
Fig. 15: the tip proceeds up to the splenic flexure
Fig. 16: air aspiration achieves further progression of the scope
Fig. 17: the gradual left angulation of the tip flattens the splenic fold
Fig. 18: increasing the left angulation and deflecting the tip downward while rotating the shaft to the left the tip of the scope proceeds into the distal transverse colon
Fig. 19: hooking the proximal edge of the splenic fold and subsequently releasing the tip, the colonoscope enters the transverse colon