Four Handed Intubation Technique – Part 1
PREMISE
The vast majority of expert endoscopist, both Western and Eastern, adopts the single-handed colonic intubation technique, otherwise labeled “two-hands”, i.e. the operator handles the colonoscope on his/her own during the whole procedure. Only a minority of endoscopists, mainly in the Western countries, employs the two-handed intubation technique, otherwise called “four-hands”, meaning that a colleague or a nurse assist the operator in the colonic intubation.
Supporters of the 2-hands technique underscore that it guarantees a better control of the colonoscope movements during intubation compared to the 4-hand technique. Seminal studies in the West by two fathers of colonoscopy such as Jerome Waye and Christopher Williams have largely contributed to the widespread application of the 2-hands technique. They have highlighted that the 4-hands technique is inadvisable because it is clumsy and reduces the perception to the maneuvers of the operator. Moreover, while in previous decades a number of publications have described in details how to correctly perform a 2-hands colonoscopy, there are scant data in the literature on how to technically perform a 4-hands colonoscopy.
Recently, it has been reported that less than 20% of Norwegian endoscopists adopt the 4-hands technique, but this minority achieves a higher cecal intubation rate, faster and with less discomfort for the patient. In Italy there are no data on the percentage of endoscopists that use the 4-hands technique, but it could be roughly estimated to be around 40%.
Despite being considered an outdated and ineffective method, nowadays the 4-hands technique may offer a number of chances, especially in the light of the technical improvements of modern colonoscopes, provided that clear-cut modalities of performance are adopted and the interaction scenario between endoscopist and nurse is correctly interpreted.
In this section one of the authors of the website (G.G.) describes the basic principles of the 4-hands colonoscopy, based on over 30-years experience in diagnostic and therapeutic colonoscopy.
G. Gizzi, V. Villani
10 Rules for a correct 4-hands colonoscopy
1.how to organize the endoscopy room
2.how to grab the handle of the colonoscope
3.how to place the colonoscope
4.the role of the Endoscopist
5.the role of the nurse assistant
6.how to manage the patient
7.how to angle the tip of the scope
8.how to rotate the scope (torque-steering)
9.How to advance the scope: 'passive bending' and 'active bending'
10.How to retract and straighten the scope
1. The Endoscopic Room
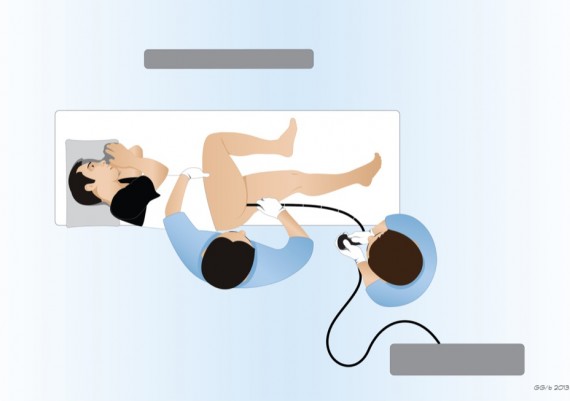
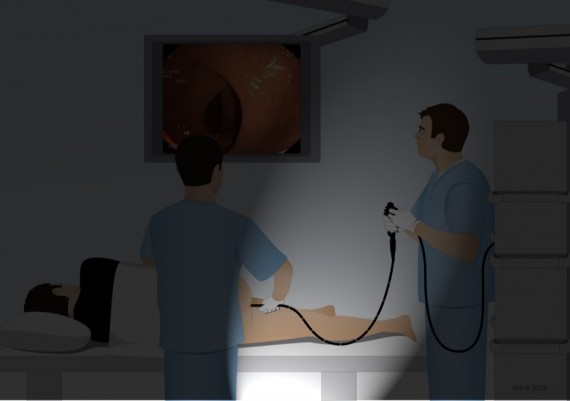
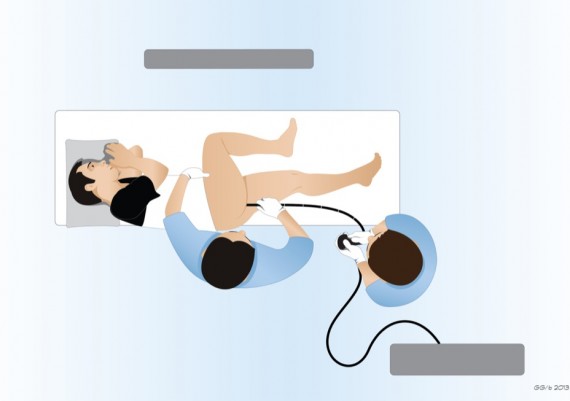
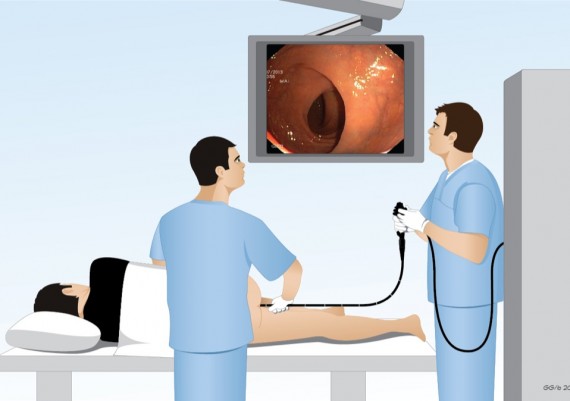
The endoscopic room should be sufficiently large to allow a functional interaction between the operator and the nurse. The position of the endoscopist and the nurse in respect to the endoscopic table, the instrument rack and main monitor is essential to perform the colonoscopy insertion maneuvers (Fig. 1).
Fig. 1: endoscopists adopting the 4-hands technique should predispose a functional scenario for the interaction with the nurse assistant. The endoscopic table should be in front of the operator(s) to secure the rectilinear position of the colonoscope. The principal monitor should be located on the right, while an accessory monitor can be located on the left, so that if the endoscopist rotates the chest, he/she can always have a frontal view of endoscopic image. The instrument rack should be on the left of the operator and at the back of the nurse and should be moved back and forth during the procedure so as not to create excess traction on the connection between scope handle and light source, and not to limit the movements of the endoscopists.
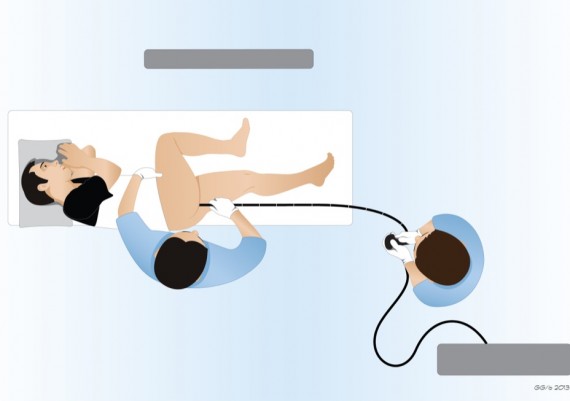
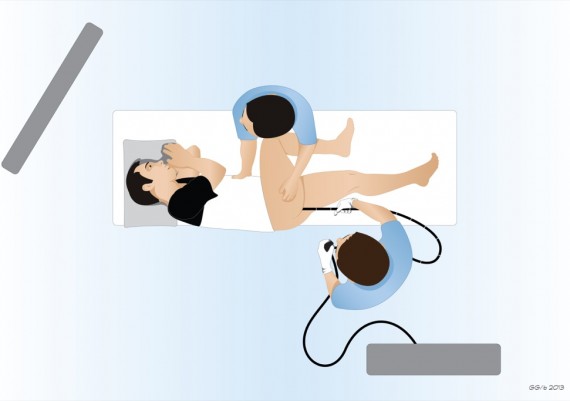
Harmonious layout of this scenario’s components facilitates all the maneuvers of both the operator and the nurse assistant (Fig. 2 A-B)
Fig. 2 A-B: endoscopic room in the 4-hands colonoscopy from above (A) and in perspective (B). The patient’s table is located at the center of the room. At the beginning of the procedure the patients lays on the left side decubitus. The main monitor is located in front of both operators and easily accessible for their view. During the procedure it can be moved according to specific needs. The nurse is always at the back of the patient, on the left side of the table, unlike the single-handed colonoscopy technique. The endoscopist is at the foot of the table, at an adequate distance to keep the scope straight. The instrument rack is at the left of the operator, with a 90° angle (to be kept constant during the procedure), so that the connection between the scope handle and the light source rack would allow any chest rotation without excess traction.
2. How to grab the handle of the colonoscope
The handle of the colonoscope should be grabbed with the left hand, soon below the control knobs, while the right handle operates the “left-right” knob, the aspiration button and the accessory switches. A correct grip is essential to achieve an easy and fine-tuned angulation of the tip of the scope. The endoscopist using the two-hands technique employs a left-handed grip in which the handle is leant on the hollow between the thumb and the index with the middle finger, the annular and the little finger, while the thumb and the index operate the up-down control knob (fig. 3).
Fig. 3: how to grab the handle in the 2-hands technique. The thumb (1) maneuvers the up-down knob, the index (2) operates insufflation and lens washing (and activates the above-placed freeze frame switch when needed); The remaining three fingers (3,4 and 5) hold the scope leant on the palm of the left hands and in the hollow between thumb and index; the middle finger (3) can also operate the left-right knob helping the thumb which can slide in opposition, or upward on the aspiration control button.
The arm is kept on the left of the endoscopist’s body to avoid hindering the right hand which is busy in the insertion-extraction and rotation of the shaft of the colonoscope (Fig. 4).
Fig. 4: in the 2-hands technique, the operator (in the picture Prof. Kashida), grabs the handle of the colonoscope with his left hand, positioned on the left of the body to avoid hindering the right hand busy with insertion, extraction and rotation of the shaft of the scope.
When using the modern colonoscopes, the use of the left hand only can result in difficult activation of the remote switches at the edge of the scope handle (NBI, enhancement, etc). The endoscopist that employs the 4-hands technique grabs steadily the handle between the palm of the left hand and the three inferior fingers (middle finger, annular and little finger), practically never taken away, slightly further down compared to the operator who employs the 2-hands technique (Fig. 5).
This allows to place the index on the insufflation-washing button, and maneuver easily the thumb to operate the up-down control knob. The right hand turns the left-right knob with thumb and index (or middle finger) (Fig. 6 A); if it is necessary to simultaneously activate insufflation and aspiration, the index (or the middle finger) moves on the dedicated control button (Fig. 6 B).
Fig. 6 A-B: in the 4-hands technique, the grab of the handle exerted with the middle finger, annular and little finger of the left hand is slightly lower than the 2-hands technique. The thumb maneuvers the up-down knob, the index operates the insufflation-washing button. The thumb and the index (or middle finger) of the right hand rotate the left-right knob, if necessary the index (or the middle finger) moves onto the aspiration button.
In the 4-hands intubation technique, the left-right knob is frequently operated, unlike the two-hands technique. However, except in some steps of the procedure, it can be operated with the thumb of the right hand only because the movements of the distal tip are seldom necessary, similarly to the thumb of the left hand that operates the up-down knob. Unlike the 2-hands technique, the handle grabbed with both hands is kept next to the sternum of the operator (Fig. 7 A-B)
Fig. 7 A-B: in the 4-hands technique, the handle grabbed the handle grabbed with both hands is kept next to the sternum of the operator.
3. How to handle the Colonscopio
The shaft of the scope, from the handle to the patients, should always be kept rectilinear. This is the basic rule in the 4-hands intubation technique (Fig. 8).
Fig. 8 A and B: in the 4-hands technique it is fundamental to keep the shaft of the scope in rectilinear position.
If the scope is straightened, all the rotations applied to the handle are evenly transmitted along the colonoscope up to the distal tip; also the up-down and left-right tip deflections operated through the control knobs placed on the scope handle are correctly modulated if the scope is constantly rectilinear (Fig. 9 A-D).
Fig. 9 A-D: when the scope is straight, the rotation of the control knobs is coherently transmitted to the distal tip: turning up the knob (A) causes elevation of the tip (B),while turning the knob in down (C) causes its deflection downward (D).
If the scope is not straight, then both twisting and angulations are “absorbed” by the curvature and are unevenly transmitted to the distal tip (Fig. 10).
Fig. 10: when the shaft is curved (A), turning the knob in the “up” position, the tip deflects toward the left.
Besides, only if the scope is straightened, it is possible to modulate the depth of the insertion performed by the nurse assistant according to the endoscopist’s intention. With a curved endoscope, the advancement of the colonoscope by the nurse cannot be negotiated by the endoscopist (Fig. 11 A-B).
Fig. 11 A-B: if the shaft of the colonoscope is not straight (A-B), the insertion of the instrument made by the nurse assistant cannot be controlled by the operator through a calibrated traction.
Last but not least, with the scope in the straight position the stiffening of the control knobs is correctly transmitted if the colonoscope is engaged in a very sharp angle, or if the tip of the instrument is stuck into a stenotic segment.
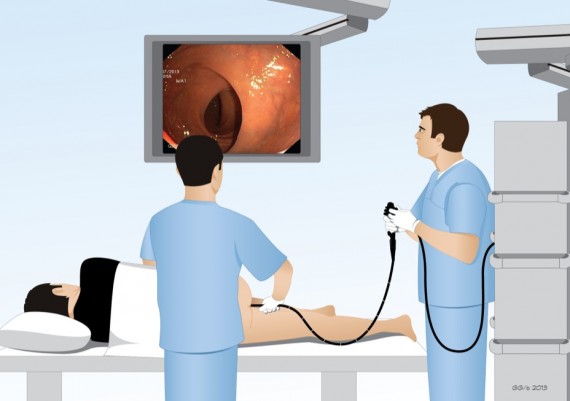
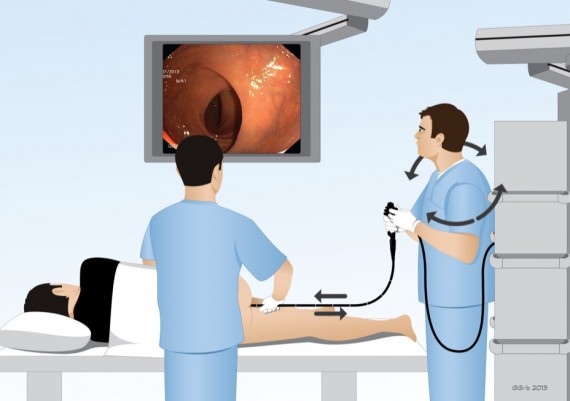
4. The role of the Endoscopist
In the 4-hands technique the endoscopists suggests the modality of scope advancement to the nurse assistant; standing upright, he or she controls the handle of the colonoscope with both hands placed in front of the sternum, rotating the chest alternatively to the left or to the right to transmit these movements to the colonoscope. Since the basic rule is that the colonoscope should be as straight as possible, at the beginning of the procedure the endoscopist is at the feet of the patient, at a distance from the table established by the length of the colonoscope itself (Fig. 12 A-B).
Fig. 12 A-B: at the beginning of the procedure the endoscopist is positioned at the feet of the patient, at a distance established by the length of the colonoscope, that should be kept as straight as possible.
The endoscopists asks the nurse to advance the scope, calibrating the depth of insertion by a gentle traction or gradually retracting the scope for the desired length; in this case the nurse “dampens” the withdrawal of the colonoscope, in order to make this maneuver harmonious and not excessively abrupt (Fig. 13 A-B).
Fig. 13 A-B: the insertion of the instrument is assigned to the nurse, instructed by the endoscopist who modulates the entity of insertion through a light traction on the scope. Since the intubation entails a number of partial withdrawal maneuvers, these are performed by the endoscopist and “dampened” by the nurse assistant.
Because the operator need to be in a stable position in respect to the patient to keep the colonoscope straight, the instrument rack should be placed on his/her left side, the table frontally and the main monitor at the right side of the table, more or less in front of the instrument rack. During the procedure, with the advancement of the colonoscope, the operator moves progressively forward to the patient’s table. Also the instrument rack moves accordingly in order to avoid any traction on the handle of the scope and guarantee the maximum mobility to the colonoscope (fig 14 A-B).
Fig. 14 A-B: during the intubation, with the advancement of the scope in the colon and subsequent reduction of the external portion of the instrument, the endoscopist moves forward to the table and the instrument rack is progressively moved forward accordingly.
If the instrument rack cannot be moved, the table will be moved toward the operator. The main monitor, placed in front of the instrument rack, should be adapted to offer easy visibility to both the operator and the nurse. To sum up, the nurse inserts the scope, while the endoscopist acts to rotate and bend the instrument; the operator guides the withdrawal, while the nurse modulates the effect
5. The role of the nurse assistant
In the 4-hands intubation technique, the nurse has to operate the insertion and withdrawal of the colonoscope with his/her right hand, tuning any obstacles in the advancement, testing the abdominal tension or applying specific compression with the left hand. In the 2-hands technique the nurse does not usually participate to the insertion maneuvers. His/her position can be indifferently on the left or on the right of the patient (fig. 15 A). In the 4-hands technique the nurse is preferably placed at the right of the patient and on the left of the endoscopist since his/her task is to advance or withdraw the colonoscope (fig. 15 B).
Fig. 15 A-B: position of the nurse in respect to the patient’s table in the 2-hands (A), and in the 4-hands technique (B).
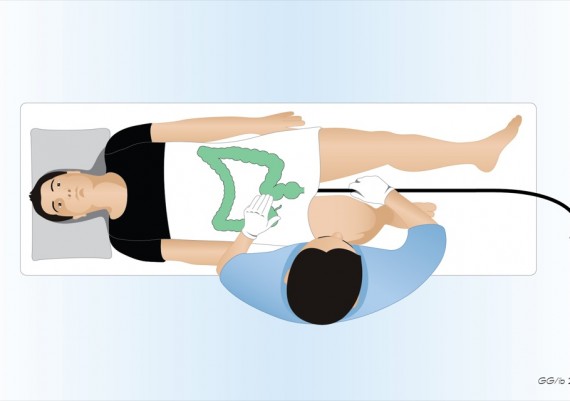
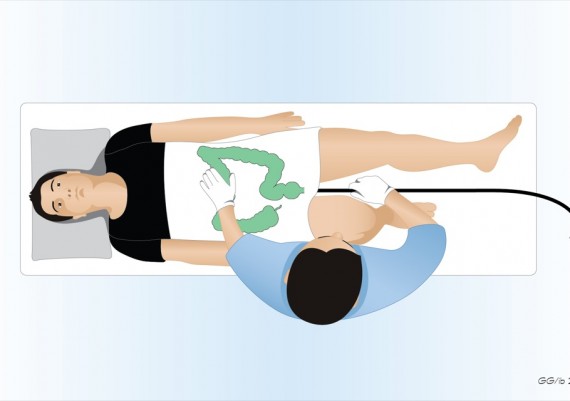
During the examination, the nurse tests with his/her hand the abdominal tension induced by the insufflation and observes any loop of the colonoscope (Fig. 16 A-B).
Fig 16 A-B: 2-hands technique: the nurse verifies the abdominal tension and detects any looping of the colonoscope
Therefore, the best position for correct operation is on the right side of the patient (Fig. 17 A-B).
Fig. 17 A-B: 4-hands technique: the nurse is placed on the same side of the endoscopist; with the right hand he/she manages the colonoscope, while the left hand is placed on the abdomen of the patient in order to verify any insufflation-induced tension or detect the presence of loops of the colonoscope.
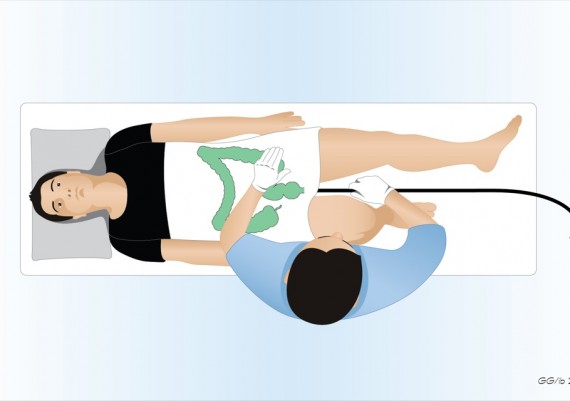
The endoscopist asks the nurse to insert the scope fine-tuning the depth of insertion through a light traction on the handle. Alternatively, the endoscopist gradually retracts the scope for the desired length, while the nurse “dampens” the withdrawal of the instrument to ensure that the maneuver is harmonious and not excessively abrupt (Fig. 18).
Fig. 18: the nurse advances and retracts the colonoscope with his/her right hand according to the indications of the operator, consistently with the images on the video monitor.
The nurse does not apply any torque on the shaft, but rather verifies the abdominal tension with his/her left hand while assessing any loop of the colonoscope. If asked by the endoscopist, the nurse exerts specific compression on the abdomen of the patient to reduce or limit possible loops of the colonoscope (Fig. 19 A-B). The standard points of compression are the sigmoid colon (Fig. 19 A) and transverse colon (19 B); compression should be exerted after the retraction of the scope for the entire length of redundant advancement.
Fig. 19 A-B: the specific points of compression on the abdomen are the recto-sigmoid junction (on the left) and the medial portion of the transverse colon (on the right).
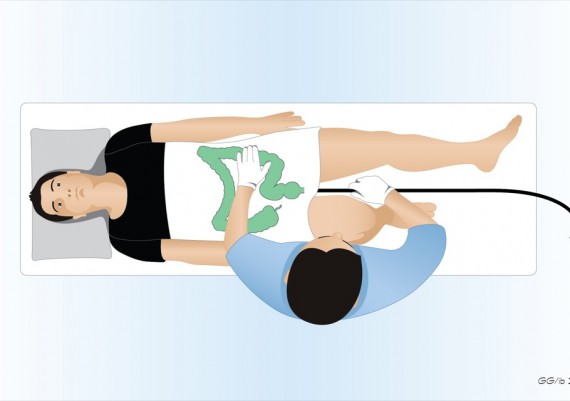
The compression performed by the nurse can also be aspecific, i.e. attempted in those sites where it may result effective in facilitating the advancement of the colonoscope (Fig. 20 A- B).
Fig. 20 A-B: the aspecific compression of the abdomen by the nurse consists of finding the proper area where the maneuver would facilitate the advancement of the scope.