Overcoming the Transverse Colon
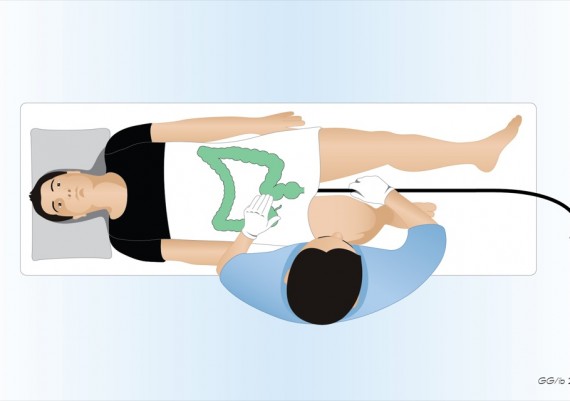
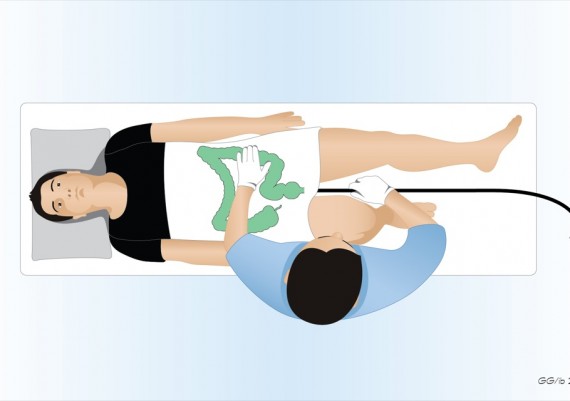
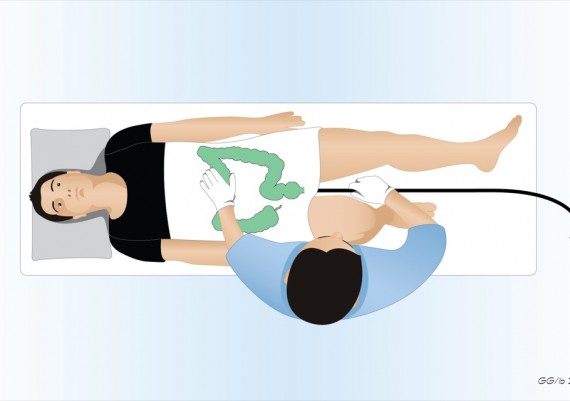
Once the splenic flexure is passed, the patient is usually rotated to the supine position because this rounds out the splenic curve and reduces the gravity negatively affecting the advancement. This position also eases the maneuvers of manual compression on the abdomen exerted by the nurse (fig. 1).
Fig. 1: the supine position of the patient favors the progression of the scope in the transverse colon
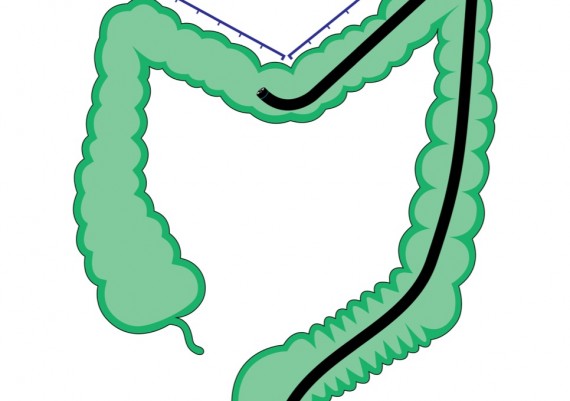
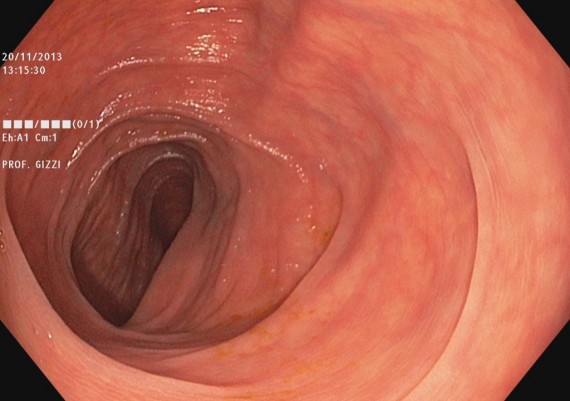
If the endoscopist has correctly straightened the sigmoid, then the colonoscope progresses easily through the distal transverse (Fig. 2), up to the apex rejoining the two branches of the arch.
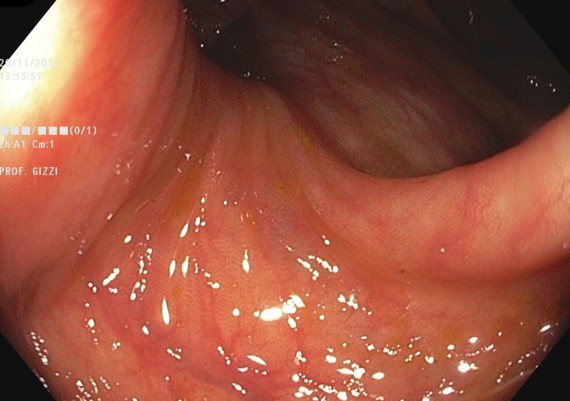
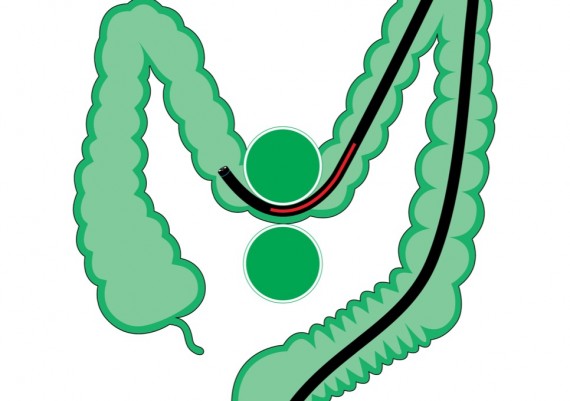
When the tip of the scope is engaged in this segment, a progressive resistance is felt to the pushing force with a reduction of the one-to-one effect (Fig. 3).
Fig. 3: when the tip of the colonoscope is engaged in the apex of the transverse arch, the resistance to the advancement increases.
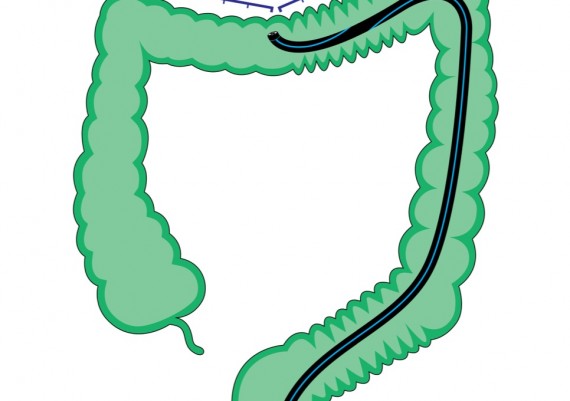
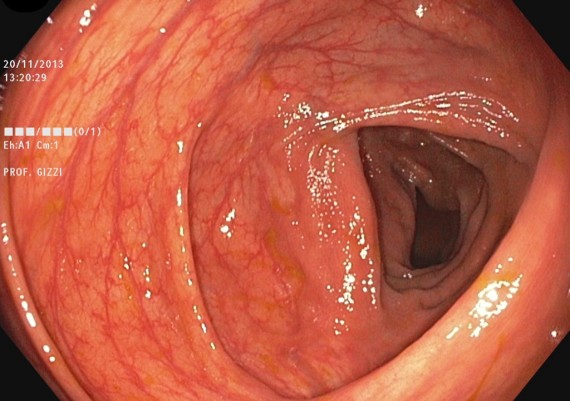
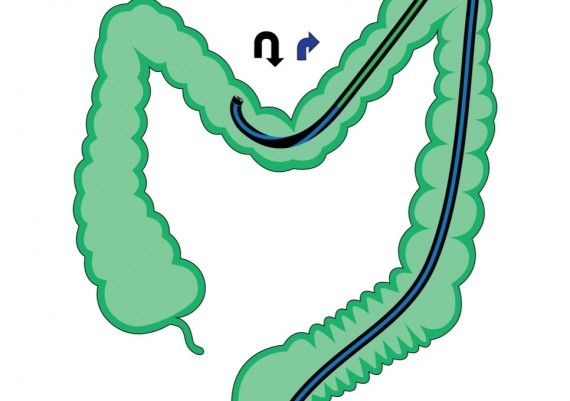
Now the objective of the endoscopist is to shorten and straighten the transverse colon. This can be achieved by a rotation of the control knobs to the right in order to strongly bend the tip of the scope to the right (and hook the colon), while simultaneously pulling back and slightly right-steering the shaft of the colonoscope (Fig. 4)
Fig. 4: shortening and straightening of the transverse colon: a) right deflection of the tip of the scope (blue arrow), b) right steering and c) simultaneous retraction of the colonoscope (red arrow) [pull-back maneuver].
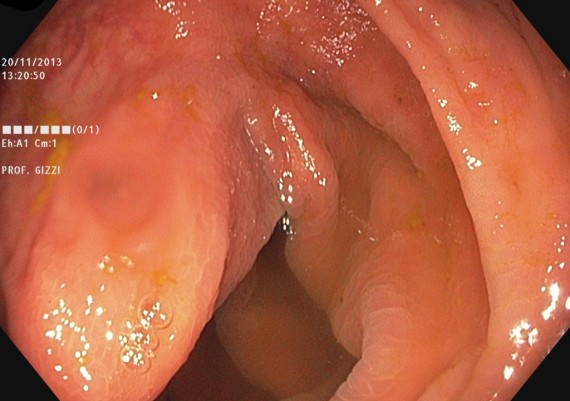
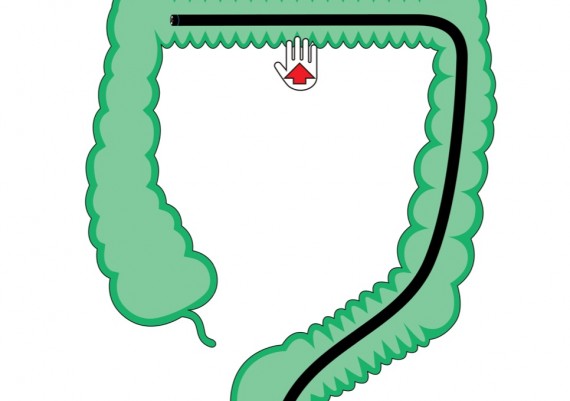
Once straightened the “V” of the transverse colon and hence achieved its shortening, the configuration of the transverse colon can be stabilized through a nurse-assisted hand pressure on the sovra-umbilical region (Fig. 5 A-B).
Fig. 5 A-B: the straightening of the transverse colon, achieved through the angulation and pull back maneuver can be stabilized applying a manual compression on the sovra-umbilical area (A). This specific compression keeps the transverse straight and further shortens it reducing the curve of the transverse toward the anterior abdominal wall (B).
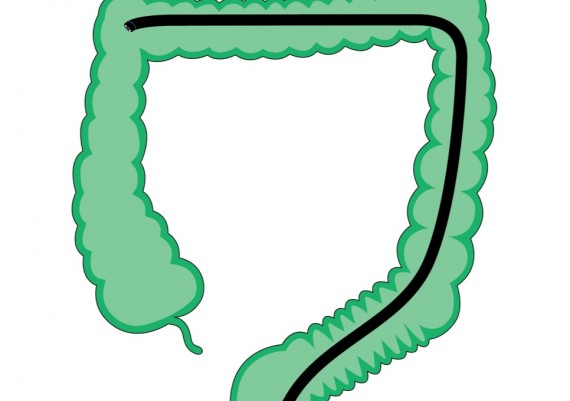
When the endoscopist releases the control knobs and stops the retraction of the scope, the tip should be free of any friction and the instrument should have regained the one-to-one effect. The simple aspiration of air will now further shorten the transverse colon, and the tip of the scope will passively approach the hepatic flexure (Fig. 6 A-B).
Fig. 6: the last maneuver to conclude the intubation of the transverse colon, provided that the previous steps have been made correctly, is to aspirate all excess air or gas. This simple trick determines a passive advancement of the tip of the scope next to the hepatic flexure, possibly aided by a slight pushing of the shaft.
The Endoscopic Sequence
Fig. 7 A-B: soon after having passed the splenic flexure, the distal portion of the transverse colon can be seen
Fig. 8 A-B: soon after the ‘V’ of the transverse colon, deflecting the tip of the scope upward, the middle portion of the transverse colon is visible
Fig. 9 A-B: through a pull-back maneuver the shortening of the colon can be obtained
Fig. 10 A-B: the manual compression below the sternum supports and increases the shortening of the colon
Fig. 11 A-B: aspiration of the air induces an automatic passive advancement of the colonoscope up to the hepatic flexure.
Transverse Ptosic Colon
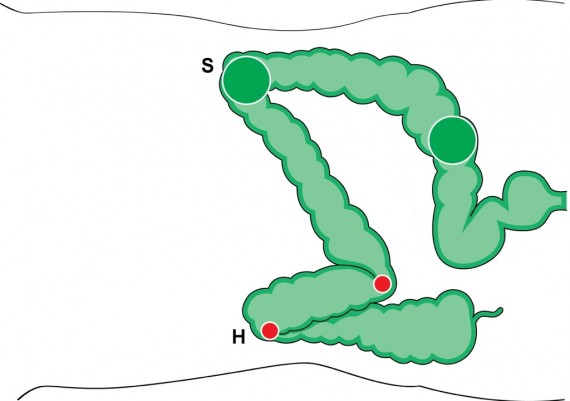
In case of a ptosic or deep transverse, the apex of the ‘V’ engages down into the pelvis and the climbing of the scope toward the proximal transverse becomes impossible because the angulation of the colonoscope tends to increase the acute angle (Fig. 12)
Fig. 12: when the colonoscope engages the apex of the curve of a ptosic transverse, the insertion force is transmitted onto a limited parietal arch (red circle), and the consequent friction prevents progression.
The colonoscope should be retracted until maximum freedom of the control knobs is perceived; if an Innoflex scope is available, the stiffness of the shaft should be increased (fig. 13).
Fig. 13: following the retraction of the scope until maximum freedom of the tip is perceived, the distal segment of the scope is stiffened (red segment).
When in maximum stiffness, the distal segment of the colonoscope is less prone to acute angulations; therefore, by pushing again toward the apex of the “V” of the transverse colon, the tip of the scope will easily proceed toward the proximal transverse, because the opened angle favors the distribution of the pressure onto a wider arch of the colonic wall and then the sliding and advancement of the colonoscope (fig. 14)
Fig. 14: stiffening of the distal segment of the colonoscope limits the excessive passive bending of the instrument when pushing on the colonic wall, and distributes more evenly the pressure onto a wider arch (green circle). This helps sliding and progression of the colonoscope.
Once passed the median portion of the transverse, the operator resets the stiffening of the scope, and performs a pull-back maneuver with simultaneous right steering and retraction of the instrument to shorten the colon (fig. 15).
Fig. 15: maneuver to shorten the transverse: bending to the right, right-steering and retraction of the scope.
Then the procedure continues with the steps already described, that are nurse-exerted manual compression below the sternum and simultaneous de-sufflation (fig. 16 A-B).
Fig. 16 A-B: the final maneuvers to end up the progression along the transverse colon are the manual compression in the region below the sternum and the aspiration of as much air or gas as possible to shorten the colon.
What to do if the progression is impossible?
When the colonoscope is stuck in the apex of the “V” of the transverse colon and does not climb upward to the hepatic flexure despite all the correct maneuvers, the possible tricks are:
1) change the site of manual compression exerted by the nurse searching for the specific point that helps progression of the scope (Fig. 17 A-B).
Fig. 17 A-B: when the scope does not progress along the transverse colon, the nurse exerts aspecific or random manual compressions on the abdomen to search for favorable effect.
2) change the position of the patient to the right lateral decubitus, so as to widen the angle of the splenic flexure and favor the advancement of the colonoscope, taking advantage of the gravity (Fig. 18 A-B)
Fig. 18 A-B: positioning the patient on the right side, the angles of the flexures are modified
3) verify the degree of stiffness of the colonoscope, and reset it (Fig. 19 A-B).
Fig. 19 A-B: if the control knob of the variable stiffness is activated, it should be reset