Anorectal Sepsis – Part 1
Introduction
Abscesses and fistulas in the anal region are common, and have a common cause; the abscess is an acute manifestation, and the fistula is a chronic condition.
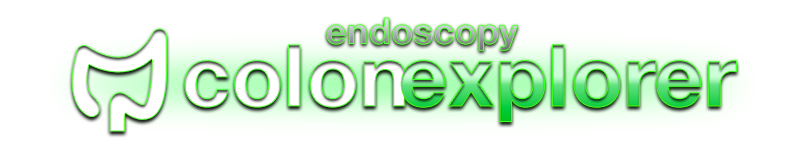
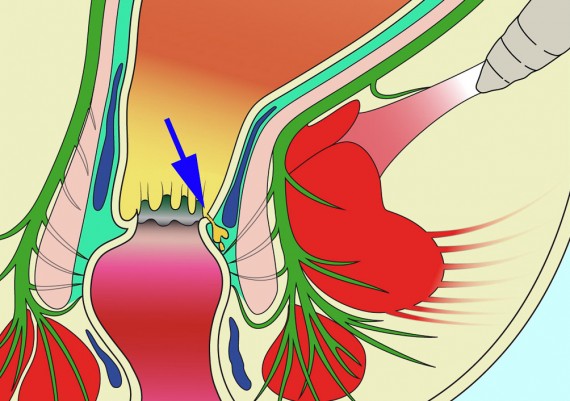
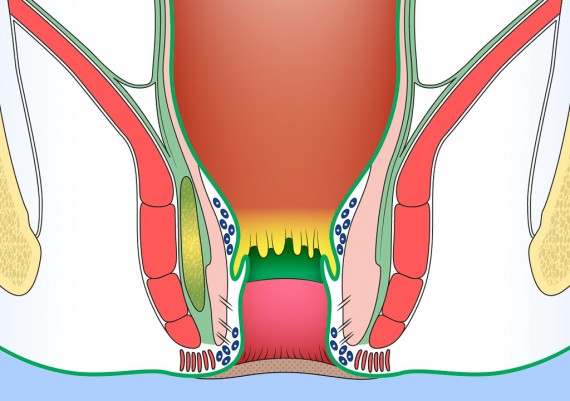
It is felt that most anal sepsis originates by the anal glands or crypts (Fig. 1) (cryptoglandular sepsis theory proposed by Eisenhammer and Parks), and this theory is supported by the fact that the primary anal orifice is found at the level of the pectinate line (Fig. 2).
Fig. 1: Anal crypts (arrows) at the level of the pecten line (endoscopic aspect with NBI technology)
Although fistula in ano may be found in association with a variety of specific conditions, the majority are classified as non-specific . Fistula in ano may be seen in association with Crohn’s disease, tuberculosis, pilonidal disease, immunocompromised patients.
Drainage of abscesses of the anal region may result in healing in > 30% of cases.
Anatomy
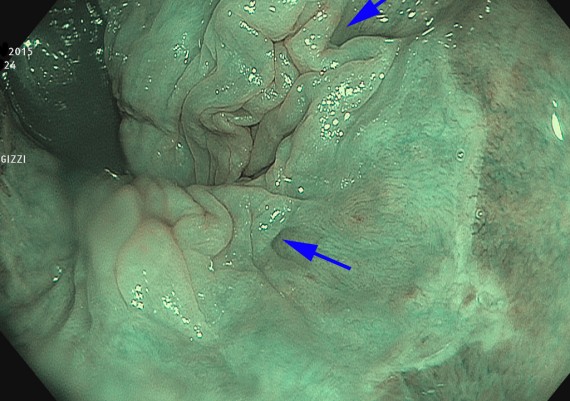
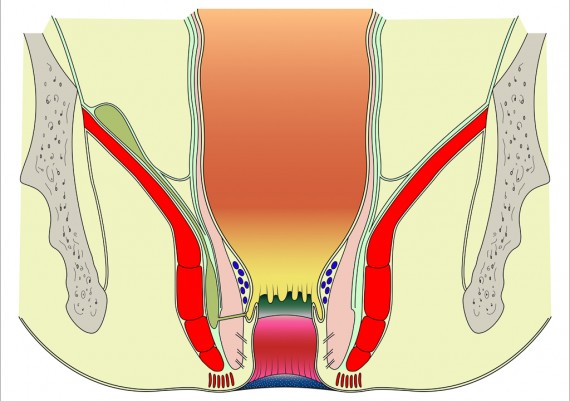
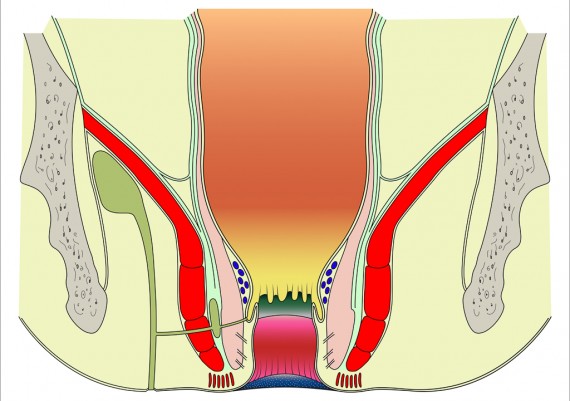
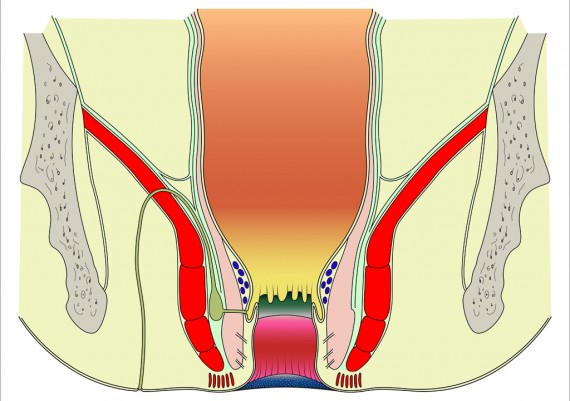
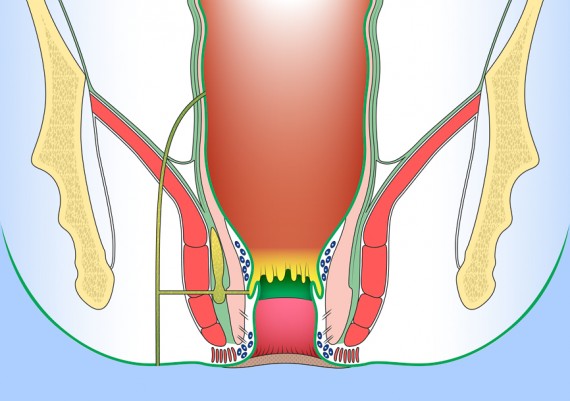
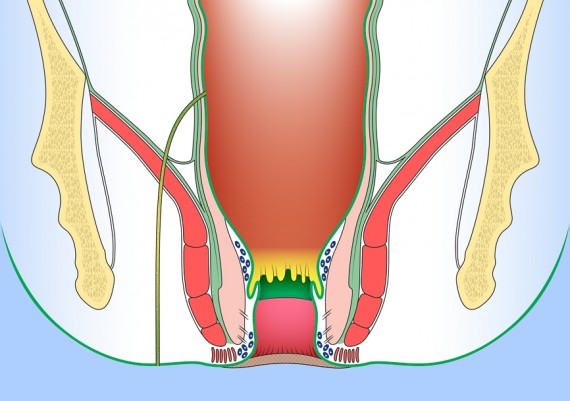
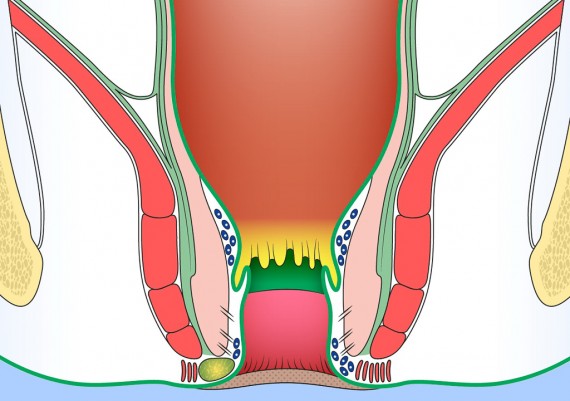
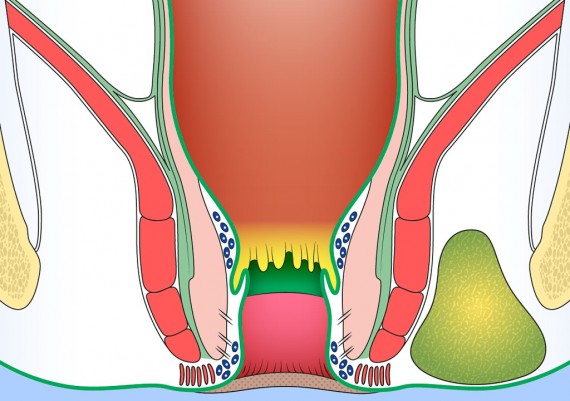
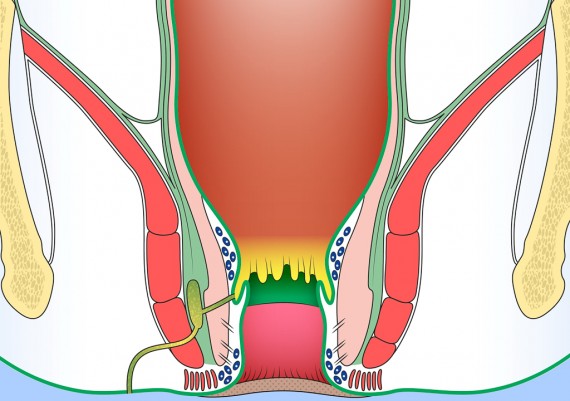
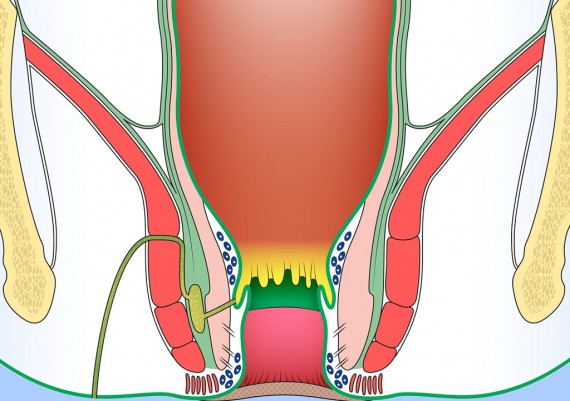
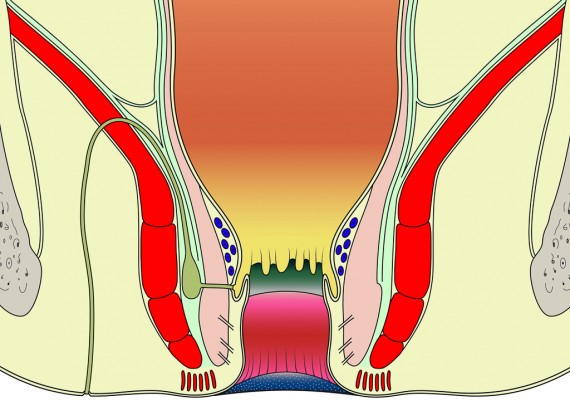
Understanding the anatomy of anal region and pelvic floor is crucial for appreciating the origin and ramifications of anal fistulas . Reduced to its simplest form, the anal region includes two funnel-shaped structures. 1) The inner structure is the lower end of the circular layer of the rectum and is referred to as the internal sphincter. 2) The outer structure is a funnel of pelvic floor muscle, formed by levator ani, puborectalis and external sphincter. Betwen the two structures is the intersphincteric plane (longitudinal layer) (Fig. 3).
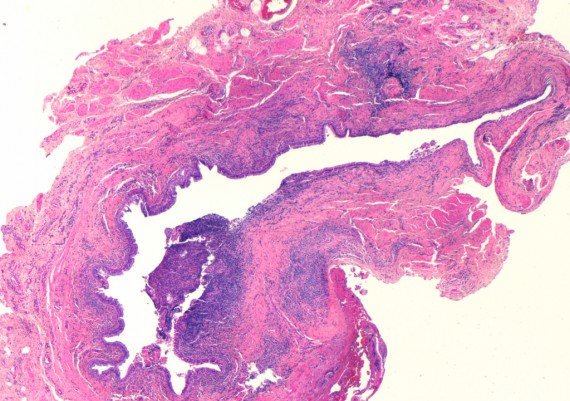
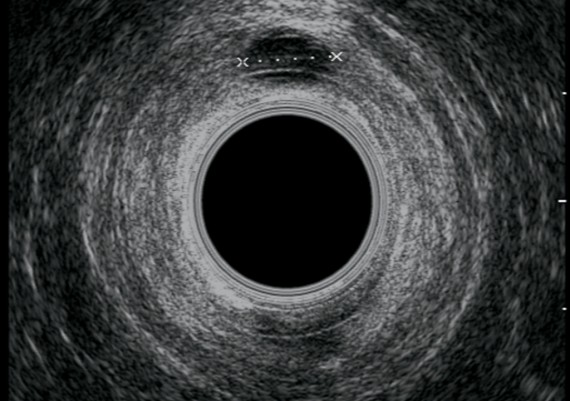
In the middle portion of the anal canal, at the level of the dentate line, the ducts of the anal glands (glands of Hermann & Desfosses) empty into the crypts (Fig. 4 A-B).
In the middle portion of the anal canal, at the level of the dentate line, the ducts of the anal glands (glands of Hermann & Desfosses) empty into the crypts (Fig. 4 A-B).
Diarrhoea, anal canal inflammation or infection may lead to edema and blokage of the duct, resulting in cystic dilatation of the glands. Superadded infection leads to sepsis and abscess formation within the intersphincteric plane. This may track inferiorly to realize an anal margin abscess; if it tracks through the external anal sphincter an ischiorectal abscess forms. The superior extension leads to development of a supralevator abscess.
Perianal Spaces and Locations of Anorectal Abscesses
Patients with abscesses around the anus typically present with pain, swelling and redness over the affected area. The anorectal abscesses can also present in confusing ways, without external manifestations.
The lateral decubitus position may be preferred for examination of anal region, because it is simple and more comfortable for the patient.
Thorough understanding of anorectal anatomy greatly enables the proctologist to properly evaluate and treat abscesses and fistulas around the anus and rectum. These abscesses and fistulas are named for the spaces they they occupy and the structures they traverse.
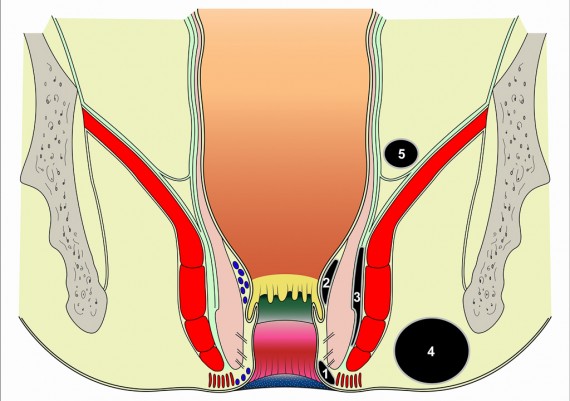
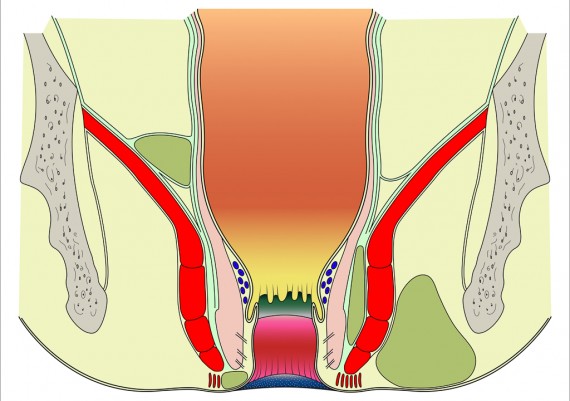
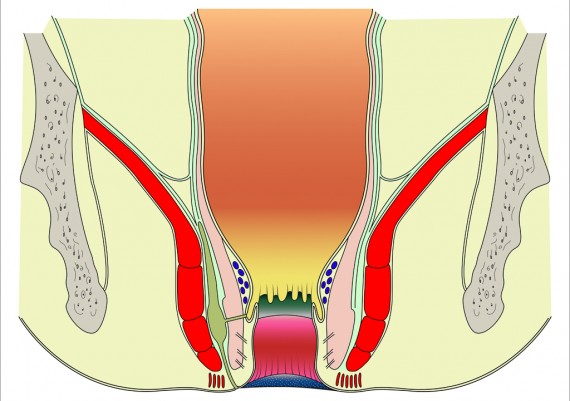
The important spaces around the anus and rectum are : 1) Subcutaneous, 2) Submucosal, 3) Intersphincteric, 4) Ischiorectal, 5) Supralevator (Fig. 5).
Fig. 5: Perianal spaces illustrating the locations of anorectal abscesses. 1) Subcutaneous, 2) Submucosal, 3) Intersphincteric, 4) Ischiorectal, 5) Supralevator
Perianal or ischiorectal abscesses manifest with obvious erythema and swelling, and perhaps fluctuance. Intersfinteric abscesses, however, hide between the internal and external anal sphincters. The patient may complain of pain, but the examiner may not see anything abnormal externally around the anus.
Similarly, supralevator abscesses are deep in the pelvis, and unless they are an extension of an abscess into the ischiorectal space, they may non present with any abnormal findings on external examination. Digital rectal examination, however, reveal an area of tenderness and fluctuance above the levator ani muscle (Fig. 6)
Fig. 6: Locations of anorectal abscesses. 1) Perianal or Anal margin, 2) Intersphincteric, 3) Ichioanal or Ischiorectal, 4) Supralevator.
Classification of Anal Fistulas
The Parks and Gordon classification is very useful to understanding the anatomy of anal fistulas. They modified the classification of anal fistulas described by Steltzner , and this is now the most widely accepted.
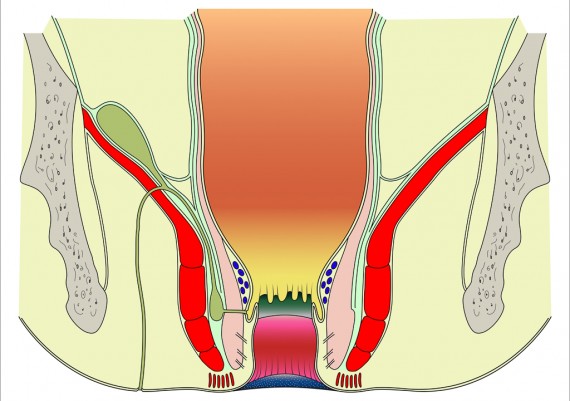
Parks identified four types of perianal fistulas: Intersphincteric, Transphincteric, Extrasphincteric and Suprasphincteric.
Intersphinteric fistulas
Intersphinteric fistulas are usually simple (Fig. 7), however, others have a blind track, or high opening into the rectum (Fig. 8).
Transphincteric Fistulas
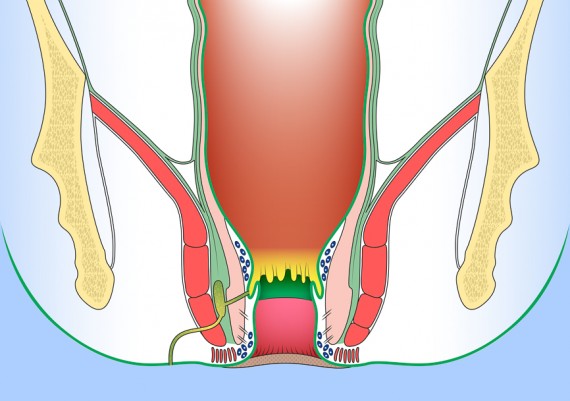
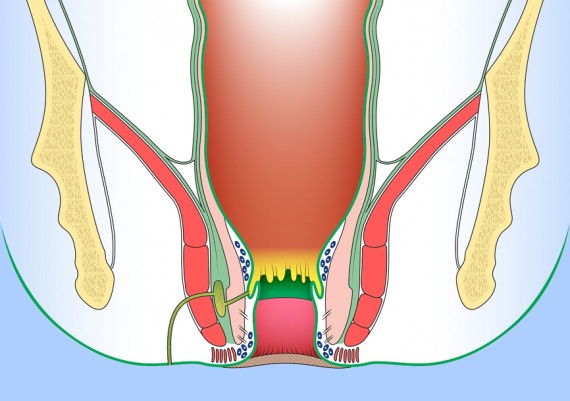
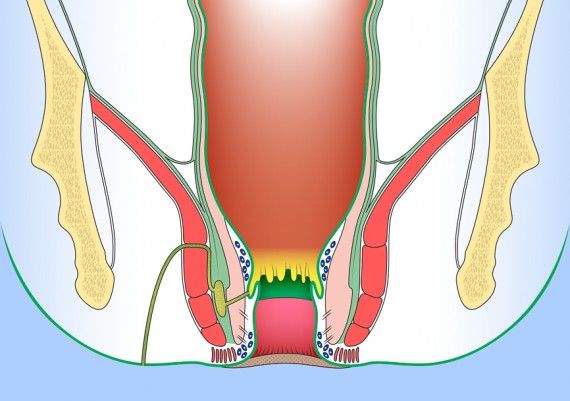
Trans-sphincteric fistulas have a primary track thath cross the external sphincter at varying levels into the ischiorectal fossa (Fig. 9-11), involving almost the entire external sphincter or only its most superficial portion. In its usual variety, and this fistula results from an ischiorectal fossa abscess.
Such fistulas may have a high blind track that may terminate below or above levator ani muscles (Fig. 12)
In the Suprasphincteric fistulas the track passes from an internal opening in the anal canal upwards in the intersphincteric plane to loop over the puborectalis and pass downwards through the levator ani to the skin (Fig. 13-14).
Extrasphincteric Fistulas
In the Extrasphincteric fistula, the track cross directly from the rectum, through the levator ani and outside the external sphincter to reach the skin. Extrasphincteric fistula may be secondary to anal fistula; a transfinteric fistula with high extension may progress spontaneously into the rectum, although tis occurrence is very rare (Fig. 15 A). Otherwise extrasphincteric fistula may be caused by iatrogenic trauma , by probe exploring tnasphincteric fistula, or secondary to specific anorectal disease ( Crohn’ disease, rectal carcinoma, chronic ulcerative colitis) (Fig. 15 B).
Fig. 15 A- B: Extrasphincteric fistula; secondary to anal fistula (A) or iatrogenic (B) pelvic disease.
Principles of Assessement
a) Identify the external opening, usually at the site of drainage of abscess (Fig. 16).
b) Identify the internal opening (usually at the dentate line) injecting air and Methilene Blue
(Fig. 17)
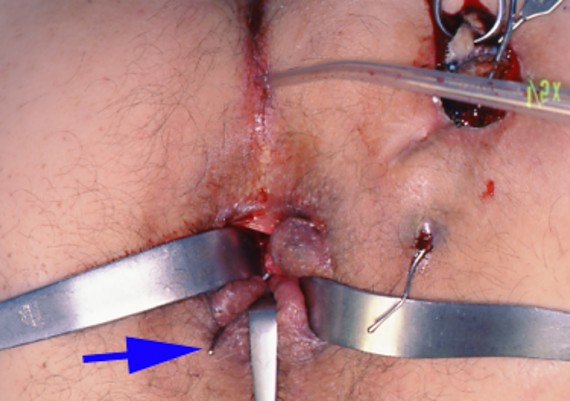
c) Outline the course of the primary tract using a probe and exclude secondary extension (Fig. 18).
Fig. 18 A-B: Two probes help to identify the primary tract (anal canal – blu arrow)) and secondary extension (right).
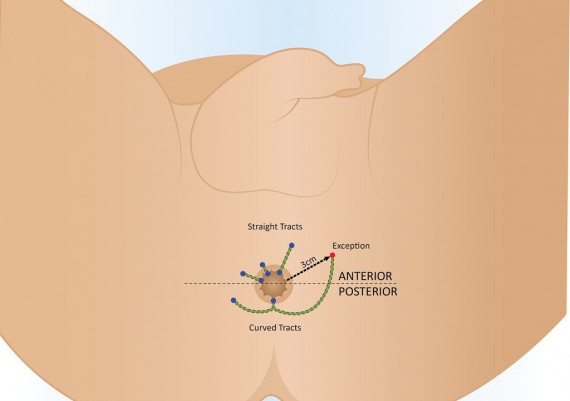
d) Goodsall rule describes the likely paths that anal fistulas of cryptoglandular origin might take based on the locations of the external openings relative to an imaginary transverse dividing line. The rule states that fistulas with an external opening anterior to a plane passing transversely through the center of the anus will follow a straight radial course to the dentate line. Fistulas with their openings posterior to this line will follow a curved course to the posterior midline (see image below). Exceptions to this rule are external openings more than 3cm from the anal verge. These almost always originate as a primary or secondary tract from the posterior midline, consistent with a previous horseshoe abscess.
Fig. 19 : Goodsall Rule is a guideline for internal opening of fistula track. Fistula can be described as anterior or posterior relating to a line drawn in the coronal plane through ischial spines across the anus, called transverse anal line.
Image below demonstrate an anterior external opening with a straight radial course to dentate line (Fig. 20)
L’immagine sottostante evidenzia l’andamento rettilineo, in direzione del canale anale, di un tragitto fistoloso con orifizio anteriore destro (Fig. 20).
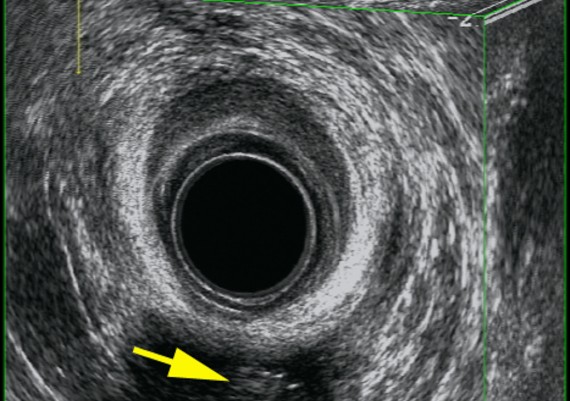
Endosonographic Imaging of Anal Sepsis
Most simple fistulae do not require imaging; fistulography has little or no place in current management of fistulae. Nowadays fistulography has been surpassed by anal endosonography (AES) and magnetic resonance imaging (MRI).
Anal endosonography is relatively cheap and easy to perform, but is operator dependent and has limited focal range, wich makes evaluation of pathology beyond the sphincters difficult to assess.
Magnetic resonance imaging is useful for identification of primary fistolous tract, and recent study reported that the sensitivity and specificity is 100% and 86% respectively. MRI is a valuable tool mainly in complex and Crohn’s related fistulae.
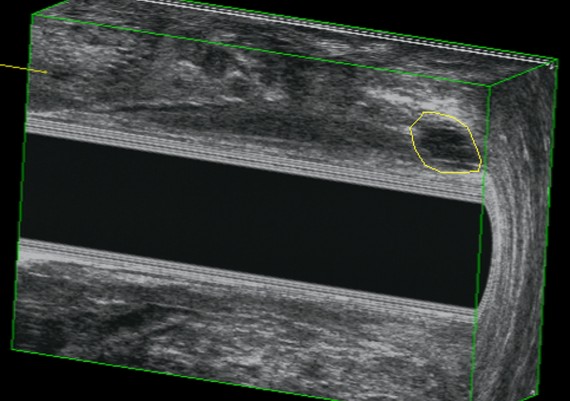
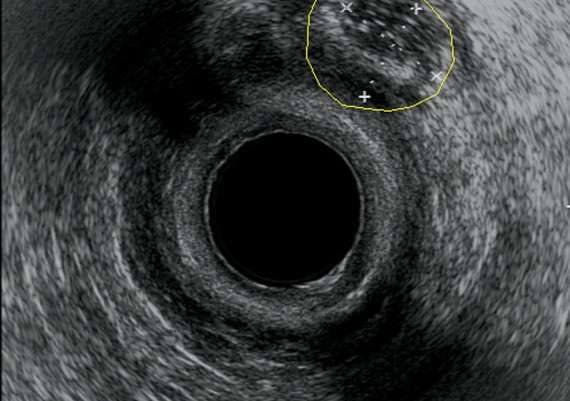
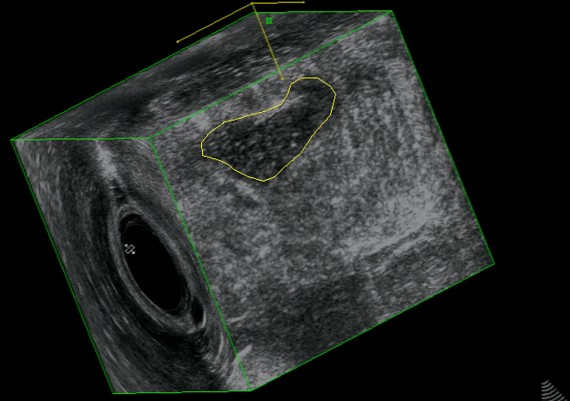
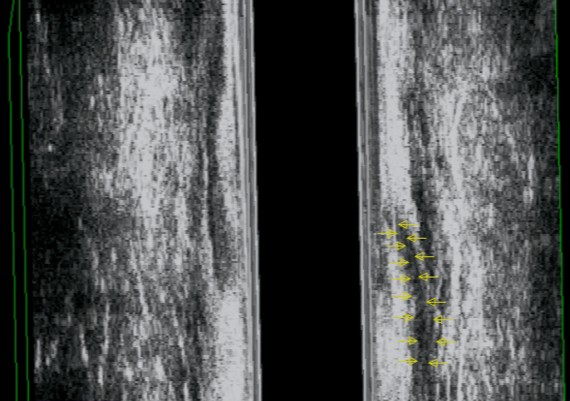
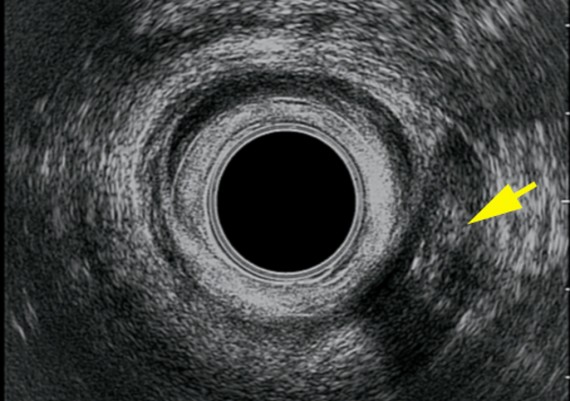
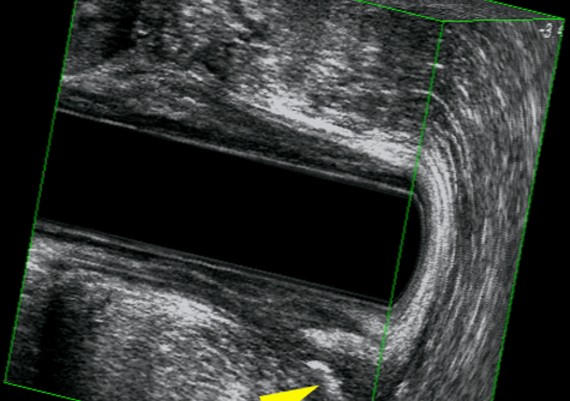
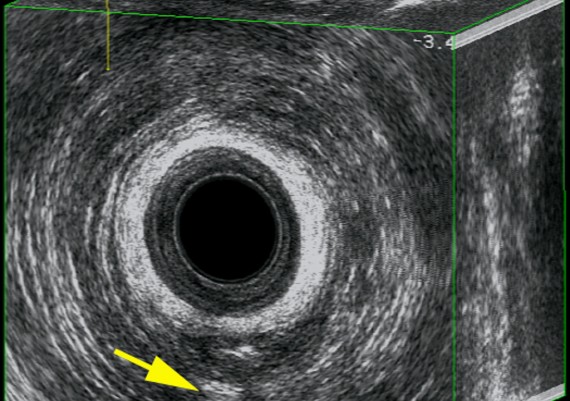
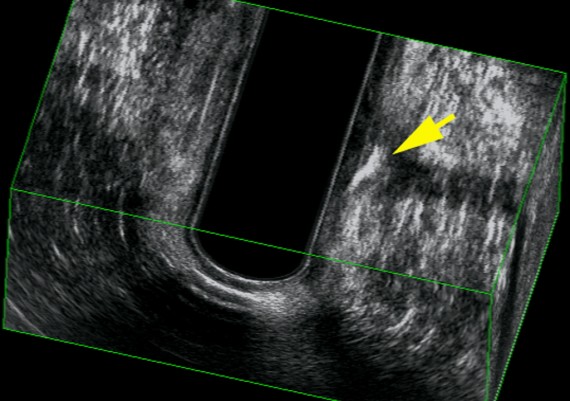
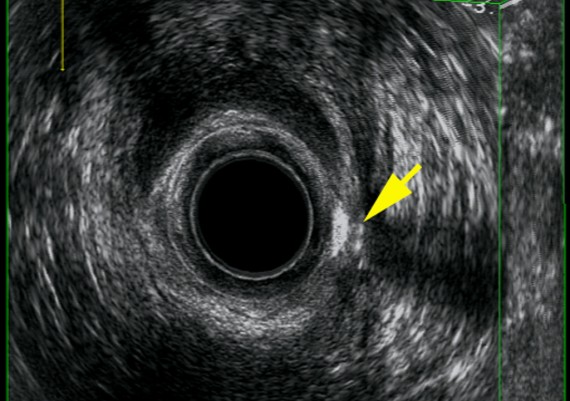
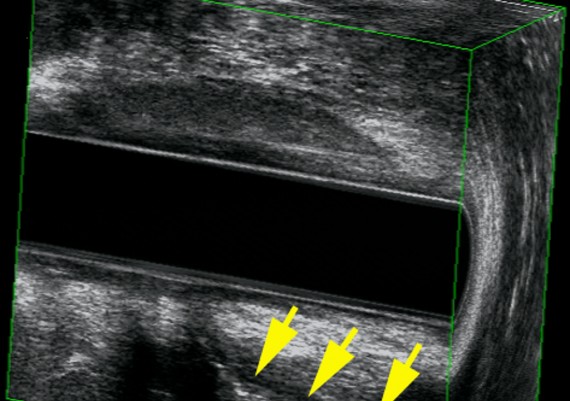
Endosonography is performed with a 10 MHz mechanically rotated transducer to give a 360° axial image. Instillation of hydrogen peroxide improves the accuracy of the technique.
Exemples of AES of perianal abscess and fistulous traks are shown in Fig.: 21-26.
Fig. 21 A-C : Anal Margin Abscess.
Fig. 22 A-C: Anterior, Ischiorectal Abscess.
Fig. 23 A-C: Intersphincteric abscess
Fig. 24 A-C : Trans - sphincteric, low Track.
Fig : 25 A-C : Trans-sphincteric high track.
Fig. : 26 A-C: Posterior, suprasphincteric track.