Colon Intubation: Morphology of the Colon and Endoscopic Intubation
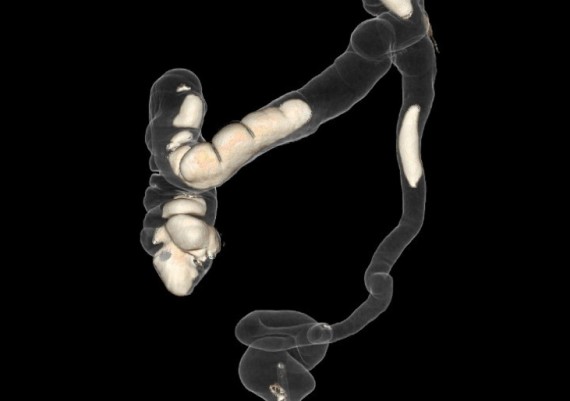
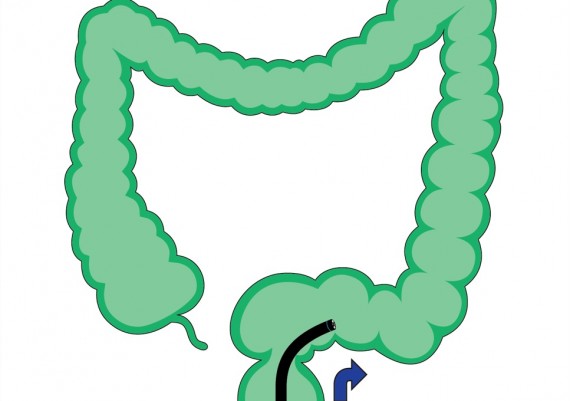
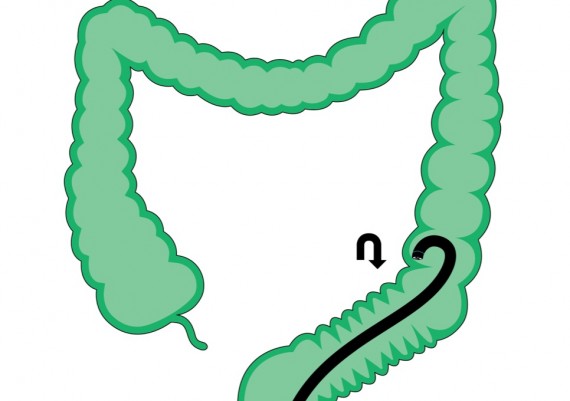
In the chapter on “Three-dimensional anatomy of the colon” we have described the arrangement of the colon within the abdomen, and particularly of those segments individually free to move (sigmoid and transverse colon). These anatomical variants entail different intubation techniques, always based on the principle that the technique should be adapted to the colon morphology, which can be modifiable only to a certain extent. As an example, a relatively less tortuous colon (Fig. 1-A) will require relatively simple straightening maneuvers to bring back the colon to a rectilinear shape (Fig. 1-B).
Fig. 1 A-B: a relatively less tortuous colon (A), both in the sigmoid and the transverse segments, allows relatively simple straightening maneuvers.
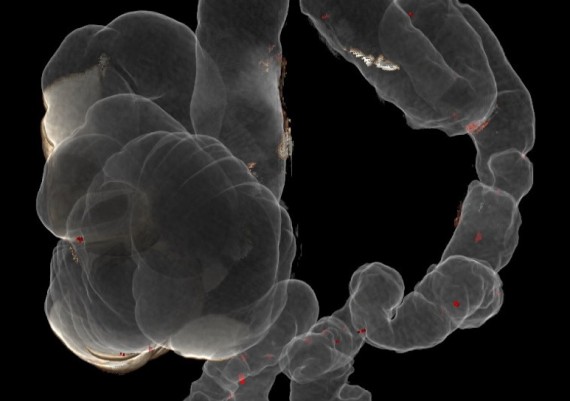
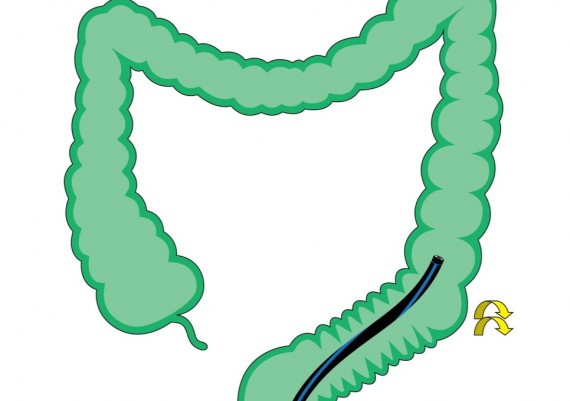
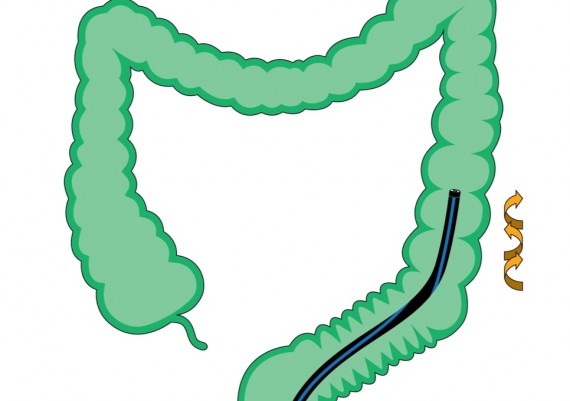
The straightening of a very redundant colon with complex sigmoid and transverse loops (Fig. 2-A), requires (Fig. 2-B) proper endoscopic ”shortening” maneuvers, joined with changes in the decubitus of the patient and specific nurse-assisted manual compressions on the abdomen.
Fig. 2 A-B: a colon with tortuous sigmoid and transverse segments (A), requires appropriate endoscopic maneuvers, changes of patient’s position on the table and specific manual compression on the abdomen to be straightened (B).
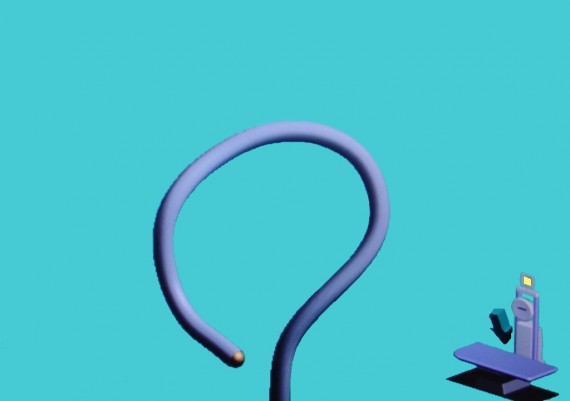
In the case of a less tortuous colon (Fig. 1), the simple “push & sliding” technique (Fig. 3 A-B), aided by changes in the decubitus of the patient and manual compression on the lower abdomen (3 B) would allow to pass the sigmoid loop and progress up to the cecum.
Fig. 3 A-B: a less tortuous sigmoid colon can be intubated with the simple “push & sliding” technique, possibly aided by a limitation of the curvature achieved by manual compression on the lower abdomen (B) to reduce the “walking stick-effect” (A).
To deal with a tortuous colon (Fig. 2), the endoscopist should master shortening and straightening basic skills, adopting case by case the pull-back and torque steering of the shaft of the colonoscope, alternating clock-wise and anti-clock-wise rotations, hooking of the distal tip of the scope on acute angles, and air aspiration to shorten the colon (Fig. 4).
Fig. 4 A-E: a particularly tortuous sigmoid colon can be passed shortening the bends, with angulation (A) and simultaneous retraction of the colon (B), torque steering to reduce residual bends (C), hooking of the tip of the scope (C) and clock-wise and anti-clock-wise rotations to fix the shaft of the scope in rectilinear position.
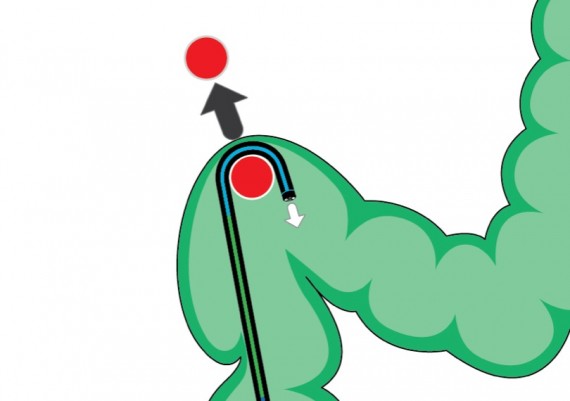
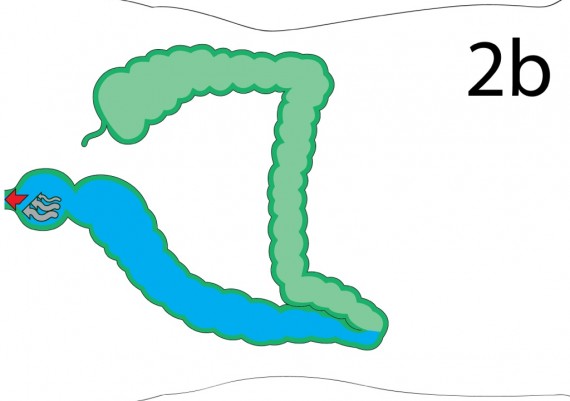
The use of variable stiffness colonoscope may be helpful to intubate colons with a tortuous sigmoid segment. This distinctive feature is usually activated after the sigmoid colon is passed with shortening maneuvers, to avoid relapse of the loop and progress to the splenic flexure. Should the attempts at straightening sigmoid loops be ineffective, the endoscopist may resort to the 'overtube' (Olympus), a 60 cm-long device inserted into the proximal part of the colon before the procedure and advanced toward the distal part to stiffen it and facilitate the progression to the splenic flexure. Other methods to overcome a difficult sigmoid colon are the use of a transparent cap on the tip of the scope (Fig. 5) and the water-immersion colonoscopy (Fig. 7).
Fig. 5: the cap placed onto the tip of the scope may facilitate the flattening of angles and facilitate progression into a very looped sigmoid.
Fig. 6 A-B: the immersion endoscopy consists into the aspiration of all the air from the lumen and the irrigation of water, which, thanks to the gravity, helps flattening the sigmoid bends and achieves progression of the straightened scope.
During the procedure the endoscopist should verify if the depth of inserted scope coincides with anatomical landmarks: 11-12 cm for the recto-sigmoid junction, 30 cm for the sigmoid-descending junction, 45-50 cm for the splenic flexure, 60-65 cm for the hepatic flexure and 75-80 cm for the cecum (Fig. 5).
Fig. 7: if the depth of the inserted colonoscope coincides with endoscopic and anatomic landmarks, it is very likely that the colonoscope is rectilinear and free from “parasite” curves.
If the length of inserted scope corresponds to these landmarks, then the operator can be confident that the colonoscope is straight, without parasite loops in the sigmoid colon or in the transverse colon.