Overcoming the Sigma – Part 1
The anatomic shape of the sigmoid colon is extremely variable among individuals; during colonoscopy the endoscopist can be challenged to deal with very different situations requiring appropriate intubation techniques.
In the “Colon 3D” chapter we report the three-dimensional morphology of the colon; it facilitates to understand how the colonoscope advances during the intubation phase, particularly at the level of the sigmoid colon.
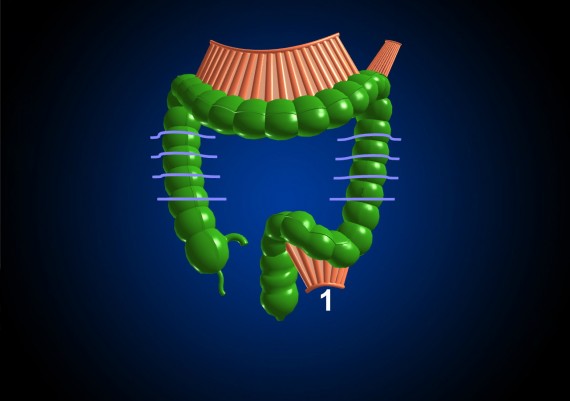
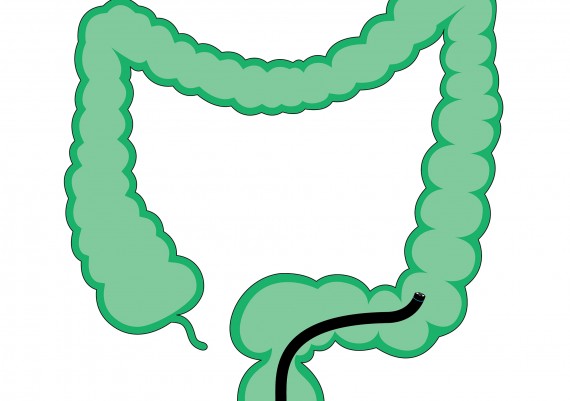
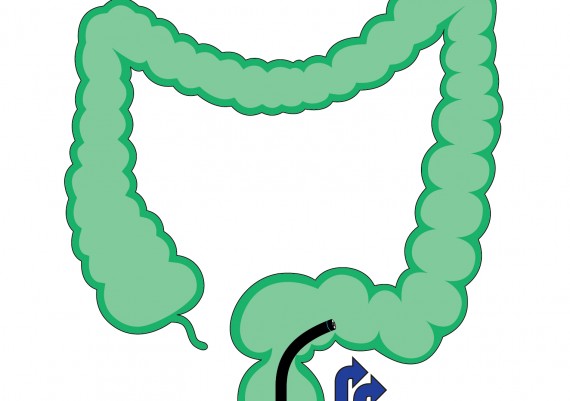
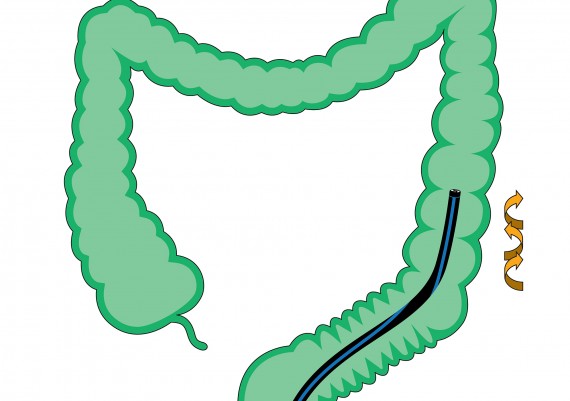
The meso-sigmoid features a “V-shaped” morphology and connects the sigmoid loop to the abdominal cavity (fig. 1).
Fig. 1: the meso-sigmod (1) has a V-shaped morphology and connects the sigmoid loop to the abdominal cavity.
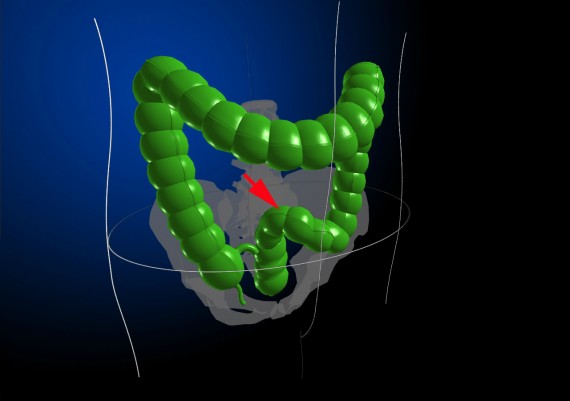
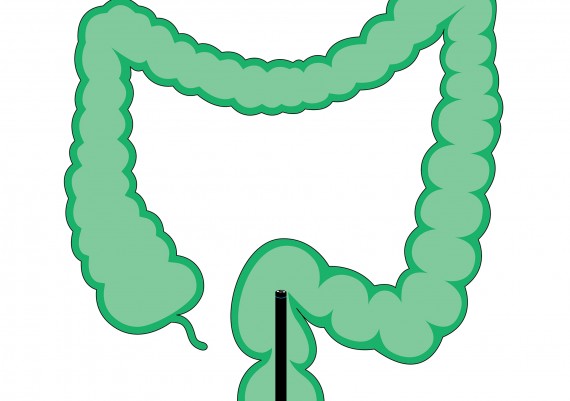
Due to the morphology of the pelvis and the anterior projection of the sacral promontory, passed the recto-sigmoid junction, the colonoscope proceeds anteriorly (toward the abdominal wall) and to the left abdominal cavity, forming the upper part of the sigmoid loop (ᔐ-top) (Fig. 2)
Fig. 2: the initial segment of the sigmoid forms the ascending branch (ᔐ-top, red arrow) of the sigmoid loop
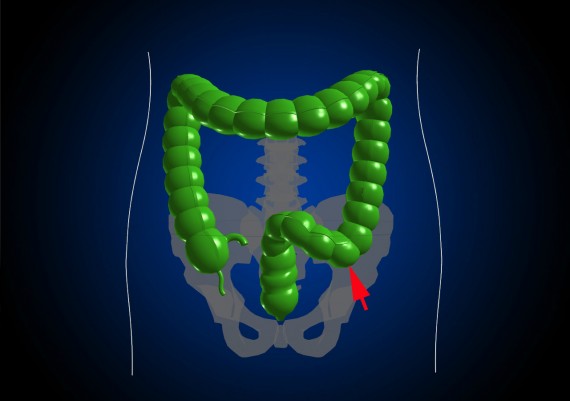
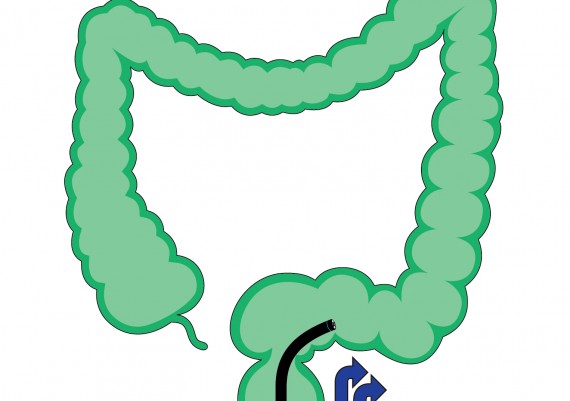
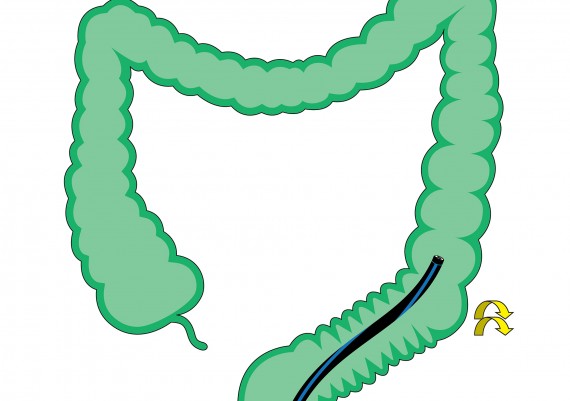
Then the sigmoid folds up posteriorly toward to left paracolic gutter, forming the inferior or descending branch (ᔐ-down) of the sigmoid loop (fig. 3).
Fig. 3: the final segment of the sigmoid, before joining the descending colon, folds up posteriorly toward the left paracolic gutter and forms the descending branch of the sigmoid loop
This morphology of the sigmoid colon is recorded in about 80% of colonoscopies, and cause the colonoscope to form a more or less pronounced clockwise spiral coil between the recto-sigmoid junction and the sigmoid-descending junction. During the intubation, the length of the sigmoid colon may vary between 40 and 80 cm, depending on the length of the meso-sigmoid and the traction exerted by the colonoscope.
When the endoscopist avoids parasite curves or strengthens them appropriately, the length of the sigmoid colon is comprised between 30 and 35 cm. Since the intubation of the sigmoid colon is the most challenging part (almost 70% of the total intubation time is spent to pass the sigmoid colon), the endoscopist should adopt all the measures to avoid excessive bends that usually tend to form in the sigmoid colon. To keep the scope as straight as possible is the way to go; otherwise, the intubation will be difficult and painful for the patient.
Anatomical variants of the sigmoid
From a practical standpoint, there are three main variants in the morphology of the sigmoid colon:
1)the short meso-sigmoid
2)the long meso-sigmoid
3)the tortuous sigmoid
Each of these configurations represents a specific condition affecting the endoscopic approach and each of these requires a combination of ancillary maneuvers to achieve a smooth and painless progression of the scope. The endoscopist does not normally know in advance the configuration of the sigmoid; therefore, he/she has to figure it out analyzing the effect and outcomes of the maneuvers employed.
Short Meso-Sigmoid
When the sigmoid colon has a short meso-sigmoid (Fig. 4), soon after the recto-sigmoid junction the endoscopist encounters more or less angled convolutions, though of relatively short extension; once these have been passed, the tip of the scope progresses rapidly to the sigmoid-descending junction. In such situations the intuibation technique requires a slow, centimeter-by- centimeter advancement, torque steering the scope after every fold and avoiding to angle the tip in excess so as not to induce the “walking-stick” effect.
Once the recto-sigmoid junction (the narrowest segment of the entire colon), has been passed, many endoscopists immediately turn the patient in supine position. With the 4-hands technique the patient can remain in the left lateral decubitus while the colonoscope, driven by the endoscopist, is advanced by the nurse.
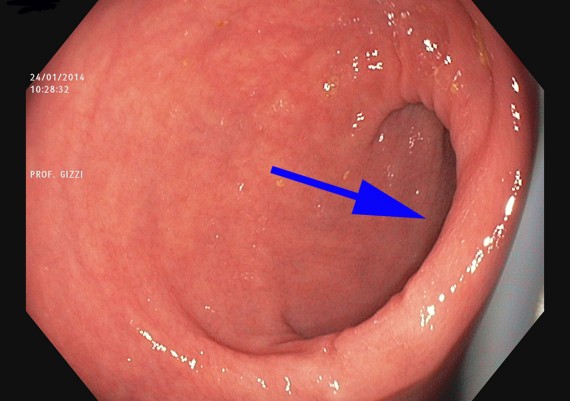
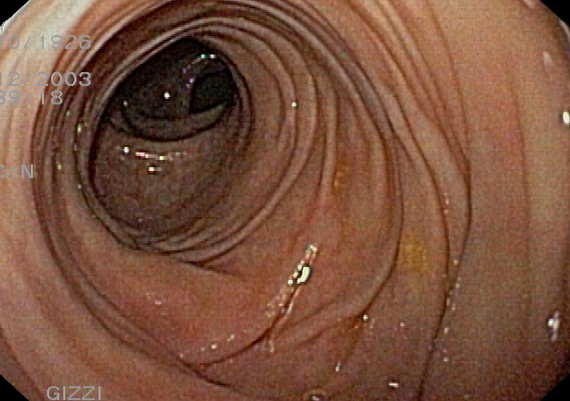
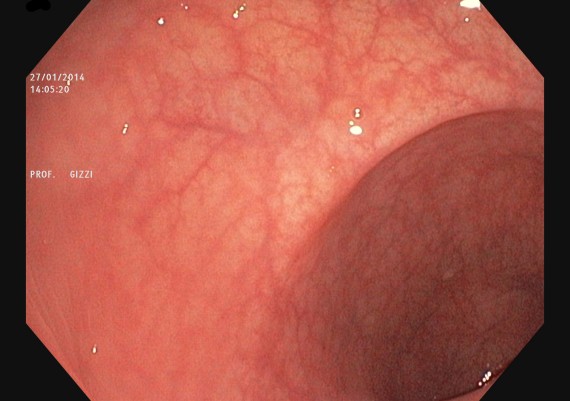
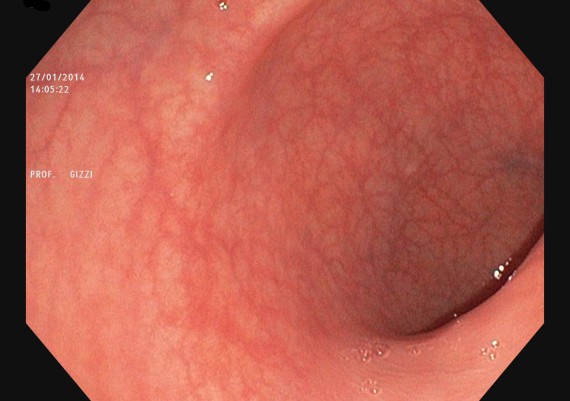
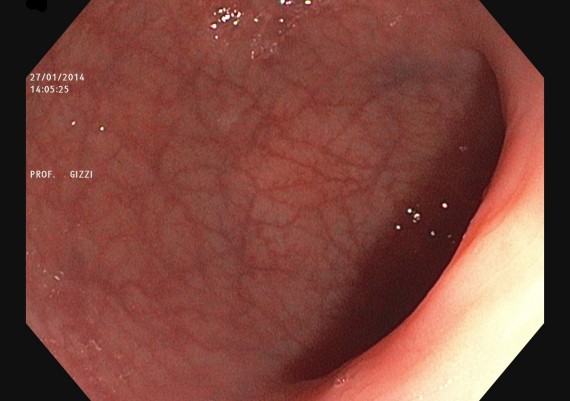
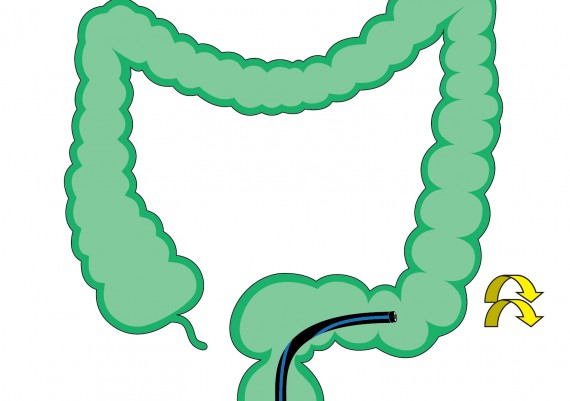
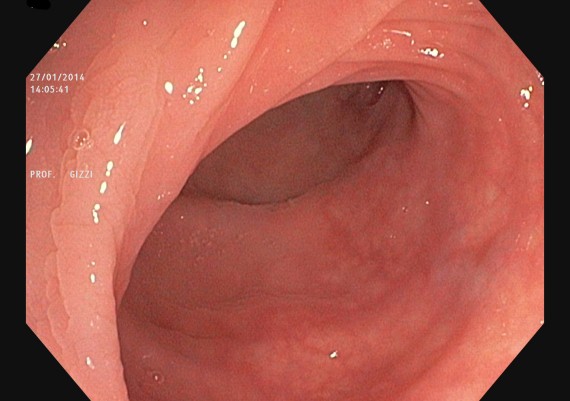
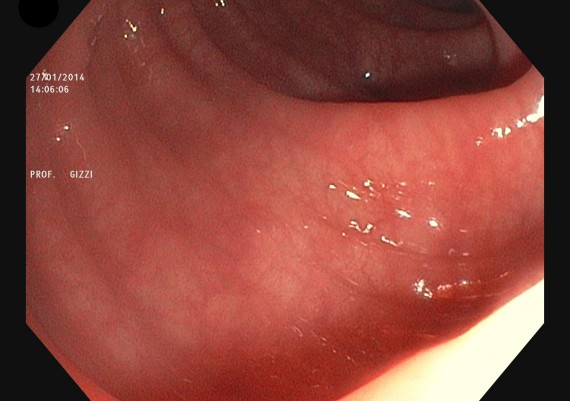
Both in the left lateral position and in supine position, the recto-sigmoid junction appears on the right of the screen (fig. 5).
Fig. 5: the recto-sigmoid junction (blue arrow) appears on the right of the screen with the patient in left lateral decubitus
The technique to pass the recto-sigmoid junction and the ascending branch of the sigmoid loop is different from that employed in the 2-hands technique. In the latter, once the tip of the scope has reached over the junction, the endoscopist starts to angle the tip toward the lumen of the sigmoid and retract the colonoscope to flatten the angle between the rectum and the sigmoid. Subsequently, torque-steering the scope clockwise with the right hand, they straighten the junction as much as possible and proceed to intubate the initial segment of the sigmoid. Keeping the scope right-rotated clockwise and with the tip at the center of the lumen, they slowly advance the colonoscope up to the sigmoid-descending junction.
In the 4-hands technique, with the patient in left lateral position, the nurse pushes the tip of the scope to reach the recto-sigmoid junction, that appears always on the right of the screen (fig. 6).
Fig. 6: in the intubation of the distal sigmoid with the 4-hands technique the tip of the scope should match the fold of the recto-sigmoid junction.
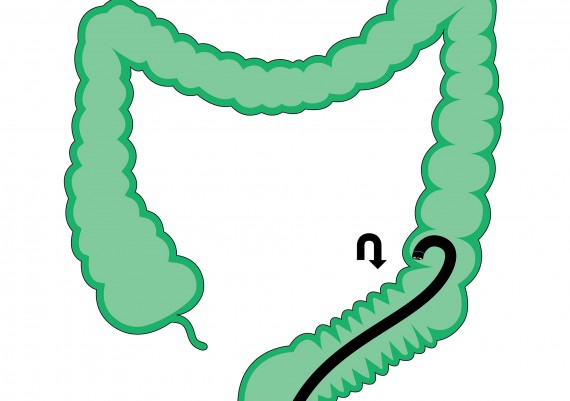
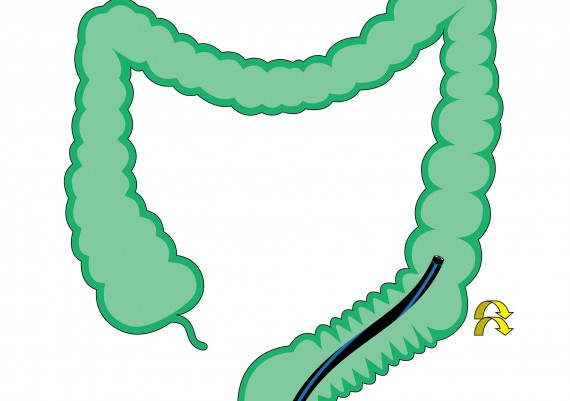
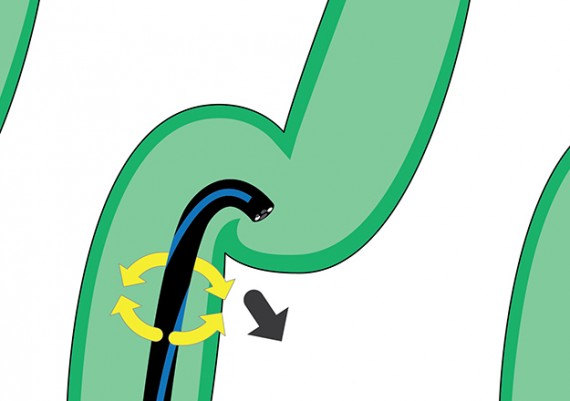
The endoscopist, with a fully straightened and slightly retracted instrument, progressively deflects the tip to the right until the limit of the knob is reached. This maneuver flattens the recto-sigmoid angle and determines an automatic progression of the tip along the superior branch of the sigmoid loop (fig. 7).
Fig. 7: the progressive and pronounced angulation of the tip to the right flattens the recto-sigmoid angle.
Always keeping the scope straight the endoscopist turns the chest to the right to transmit a 90°-degrees rotation to the tip of the scope which advances (Fig. 8 A-B) (“right turn shortening”).
Fig. 8 A-B: by rotating the chest to the right (A), the endoscopist transmits to the tip a rotation (B) that completes the flattening of the ascending branch of the sigmoid and directs the colonoscopy toward the descending branch of the sigmoid.
The segment of the colonoscope above the flexible end advances over the recto-sigmoid junction and stabilizes the obtained straightening; the tip can be released into straight position.
The colonoscope is pushed by the nurse but modulated by the endoscopist along the descending branch of the sigmoid loop, until the tip approaches the sigmoid-descending junction.
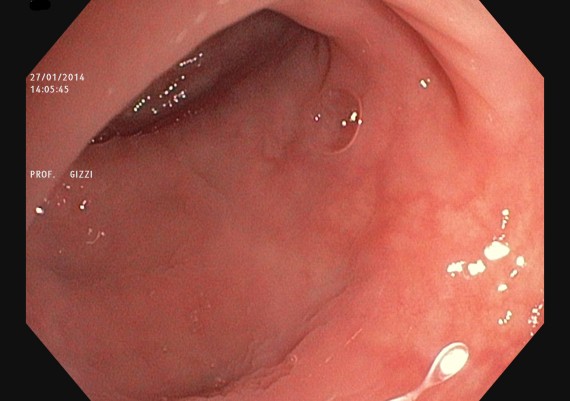
The endoscopist now “anticipates” the bend deflecting the tip to the left if the chest is still right-rotated, or upward if the operator has regained his/her normal position infront of the endoscopic table (Fig. 9).
Fig. 9: passed the descending branch of the sigmoid, the tipi s advanced toward the sigmoido-descending junction, “anticipating” the tip deflection toward the lumen.
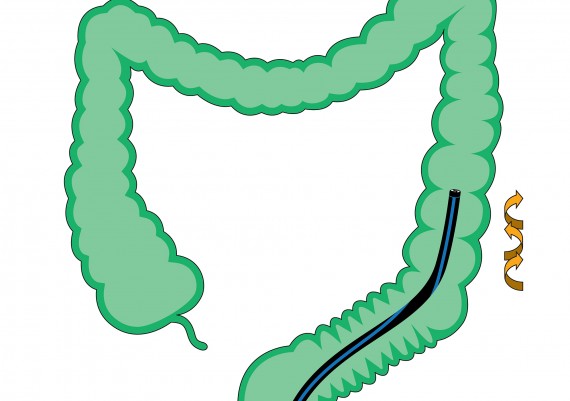
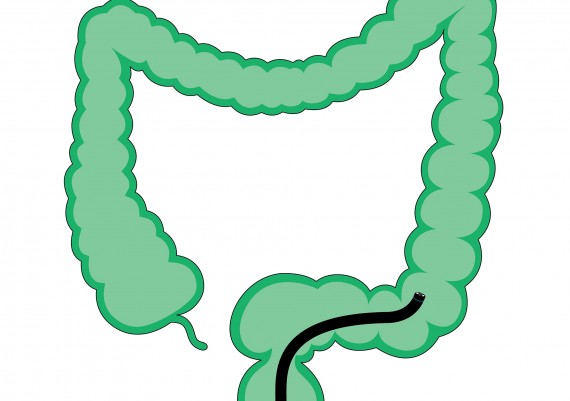
If the endoscopist feels a tension on the control knobs, i.e. the tip is still engaged in a bend, he/she rotates the chest to the right for about 90°, to complete the straightening of the scope and induce the “telescoping” of the sigmoid over the colonoscope (Fig. 10 A – B).
Fig. 10 A-B : if the shortening technique (A) is correctly performed, the sigmoid will result “telescoped” on the colonoscope (B)
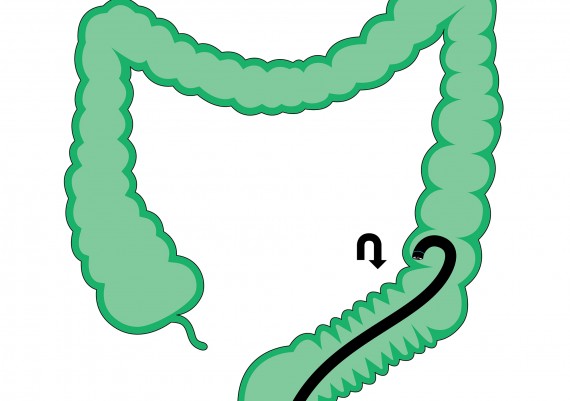
Again, stressing to the limit the tip deflection, the endoscopist hooks the fold and trails the instrument forward, until the most proximal segment of the colonoscope reaches the sigmoid-descending angle (Fig. 11).
Fig. 11: when the tip of the scope has passed the sigmoid-descending fold, the tip deflection hooks the scope to the descending colon, trails it forward straightening the distal end and places the less flexible portion of the scope over the junction.
The maneuver is completed releasing the tip free and rotating the chest to the right and to the left to transmit alternate lateral movements to the tip and stabilize the shortened and straightened sigmoid (Fig. 12 A-B).
Fig. 12 A-B: when the tip of the scope has gained the lumen of the descending colon, the alternate rotation of the chest to the left and to the right stabilise the straight position of the colonoscope.
The maneuver is completed releasing the tip free and rotating the chest to the right and to the left to transmit alternate lateral movements to the tip and stabilize the shortened and straightened sigmoid (Fig. 12 A-B).
The Endoscopic Sequence
Fig. 13 A-C: the tip of the scope is advanced over the recto-sigmoid junction (A) until the junction fold, visible on the right of the screen (B), is no longer seen. Sometimes it is possible to glimpse the lumen of the top branch of the distal sigmoid (C - blue arrow).
Fig. 14 A-D: the full deflection of the tip to the right flattens the top branch of the sigmoid and determines the advancement of the scope (B-D).
Fig. 15 A-C: rotating the chest to the right, the endoscopist transmits the rotation to the tip, which slides over the descending branch of the sigmoid; during this manever the lumen is not always visible (B – blue arrow indicates the direction of the lumen) and the endoscopist feels the sliding of the mucosa in front of tip, up to the fold of the sigmoid-descending junction (C).
Fig. 16 A-B: pushing the scope beyond the down-loop of the sigmoid, the sigmoid-descending fold can be seen (B).
Fig. 17 A-B: the rotation of the chest to the right transmits a clockwise rotation to the scope that makes the straightening of the sigmoid stable (B).
Fig. 18 A-B: as soon as the sigmoid-descending junction is passed, the endoscopist hooks the proximal side of the fold (A) to trail the colonoscope forward (B).
Fig. 19 A-B: releasing the tip free, the endoscopist rotates and contra-rotates the instrument (A) to make it stable in the lumen of the descending colon (B).
What to do when the sigmoid cannot be intubated?
When the colonoscope cannot be advanced in the sigmoid colon, and the endoscopist detects an acute angle, forcing the progression does not achieve any result, and air insufflation tends to sharpen the folds and cause pain rather than distend the bowel lumen. Since the sigmoid colon is strategic for a correct colonic intubation, it is necessary first to withdraw the scope to the junction and adopt a meticulous and calibrated advancement (“slower is faster”).
A very sharp angle, that cannot be reduced by tip deflection, may be the result of: a) severe diverticulosis; b) post-surgical adhesions; or c) pelvic engagement of the descending branch of the sigmoid loop.
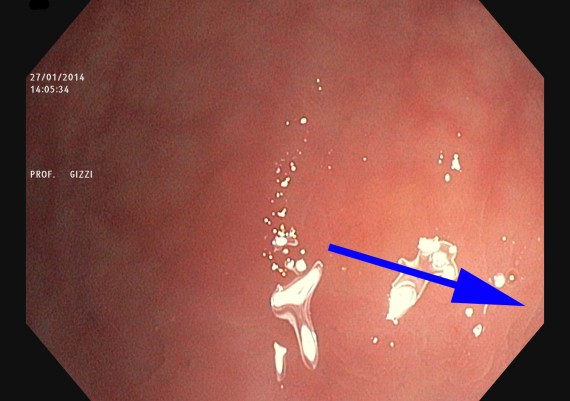
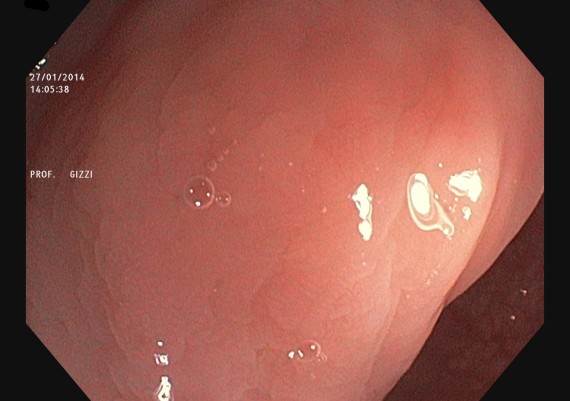
a)In the suspect of diverticular disease in the elderly, when the angulation tends to ”entrap” the tip of the scope and the changes of patient’s position are unsuccessful, the best second option is to use a pediatric colonoscope. Generally, the combination of a reduced caliber scope with the position changes results in successful advancement. Sometimes, the caliber of the sigmoid is so narrowed by peri-diverticular fibrosis, that the insufflation does not allow to see the lumen of the viscus. In such situation, with the patient preferably in the left lateral decubitus, it is advisable to adopt the “immersion technique” (Fig. 20 A-B ). This technique offers the advantage to obtain a gradual and persistent luminal distension of the segment to intubate, unlike air that accumulates in the rectum or in the proximal colonic segments.
Fig. 20 A-B: in case of sigmoid diverticulosis with pronounced luminal narrowing, the immersion technique is convenient because the instilled water endures in the colonic segment (B). The left lateral position favors the collection of water in the sigmoid colon (A).
In no other condition more than a diverticular colon with luminal sub-stenosis, does the rule of gradual progression hold true. The advancement of the scope, in fact, is achieved through tiny and repeated angulations and torsions of the tip via the control knobs or chest rotations, rather than through the pushing force exerted by the nurse. The film shows the efficacy of the immersion technique and the modality of progression through torque-steering of the colonoscope.
Diverticular Sigmoid Colon - Water Immersion Technique
Intubation of the sigmoid diverticular with narrowing of the lumen is facilitated by technical diving and the overcoming of the scrolls with alternating movements of rotation and counter-rotation.
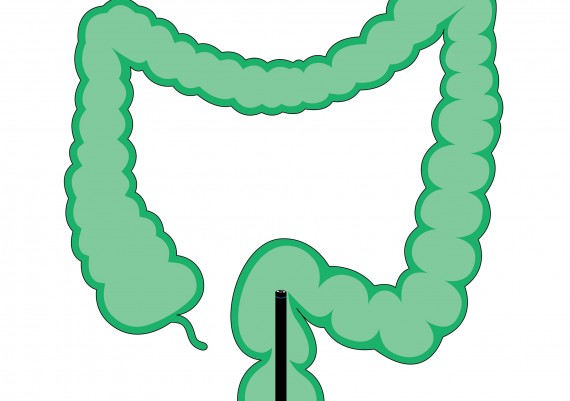
b)If the progression is awkward in patients with adhesions due to previous abdominal surgery, the first alternative is to roll the patient to the supine position, using manual compression maneuvers that facilitate the advancement of the tip of the scope. Should these maneuvers be unfruitful, the patient is moved to the right lateral decubitus, to modify the opening of the recto-sigmoid angle, provided that it is not incarcerated by abdominal adhesions. In the end, employing a pediatric colonoscope or a gastroscope, it should be tried to slowly advance past the angulations (hardly foreseeable) and adopt a technique to hook and flatten the folds (“hang on and turn over”) (Fig. 21) .
c)If the progression in the sigmoid is troublesome in very thin patients, with small pelvis, it is likely that the sigmoid loop becomes engaged in the pelvis, and therefore the tip of the scope has insufficient space to de-rotate the loops. In such situations, avoiding insufflation or aspirating excess air, it is advisable to put the patient first on his/her right lateral side, adopt the immersion technique or employ a pediatric colonoscope or a gastroscope. Once the complex sigmoid is passed, then the cecum cab be rapidly and easily reached.