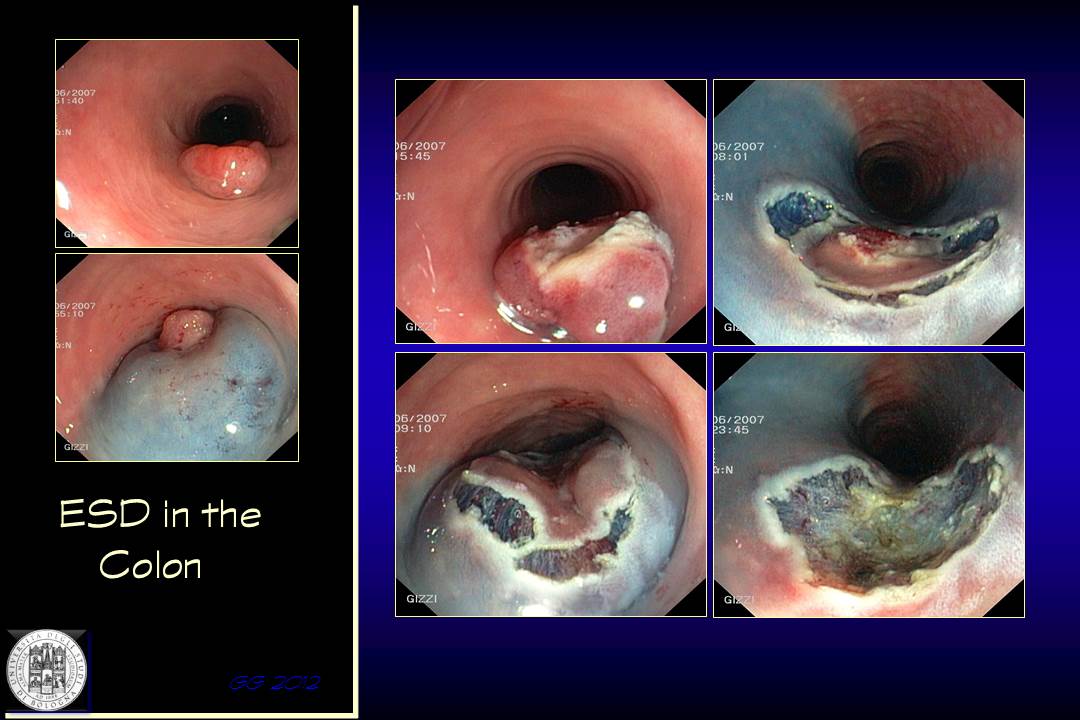
Endoscopic Staging of Superficial Neoplastic Lesions of the Colorectum
Improved quality of endoscopic imaging and refinement in endoscopic resection techniques have largely increased the potential of endotherapy of colorectal superficial neoplasia. The ability to accurately distinguish non-invasive lesions or those with superficial submucosal invasion (sm1 or sm-s) from those with deep submucosal infiltration (sm2-3 or sm-d) is crucial for the overall quality of endoscopic procedure
To establish which lesions are amenable to endoscopic resection during colonoscopy, and which specific operative technique should be employed, the endoscopist has two “diagnostic weapons” (apart from endoscopic ultrasonography which would inevitably delay the therapeutic step):
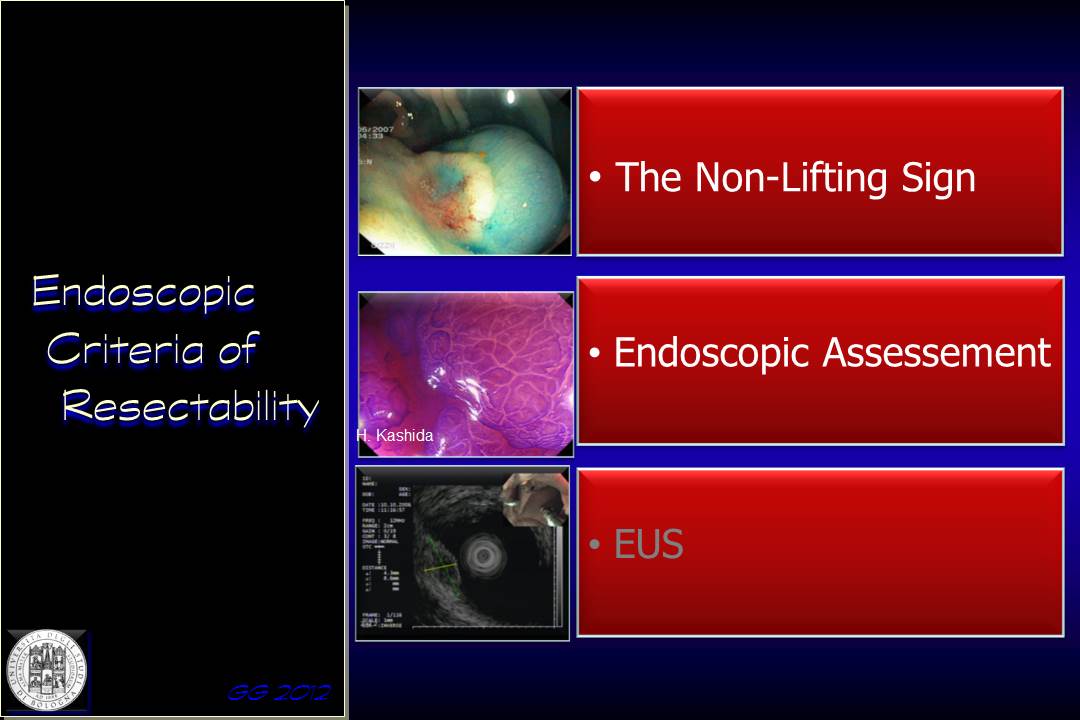
1) the ‘Non-Lifting’ sign (NLS)
2) endoscopic assessment of the lesion

Can be consider these two staging or stratification procedures as equivalent? Or, in case of complex lesions, should be adopt something more sophisticated than the NLS to select the most appropriate operative procedure?
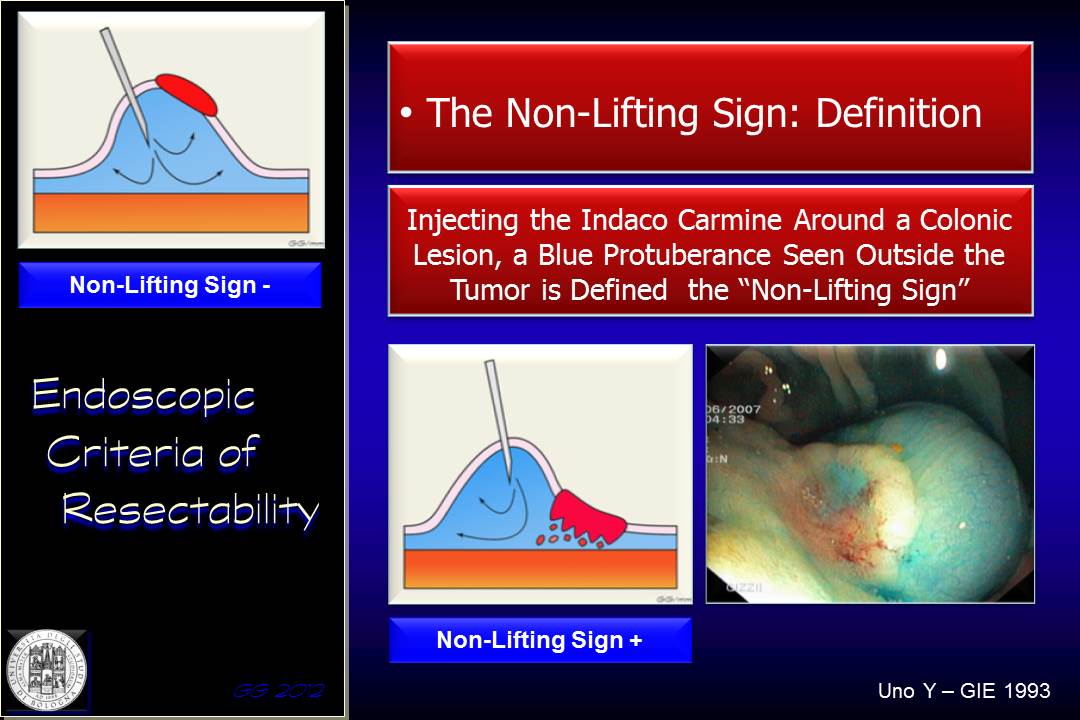
Originally described by Uno in 1993, the “non-lifting sign” is the absence of any lifting of the lesion when fluid is injected under a flat or sessile lesion in preparation for endoscopic mucosal resection (indigo carmine or originally methylene blue). The sign indicates , and a “blue cushion” occurs at the lateral margins of the lesion indicating deep submucosal invasion. This would make surgical removal of the tumour preferable to allow complete removal of the cancer. Consequently, the non-lifting sign is generally considered to be a contraindication to performing endoscopic resection.
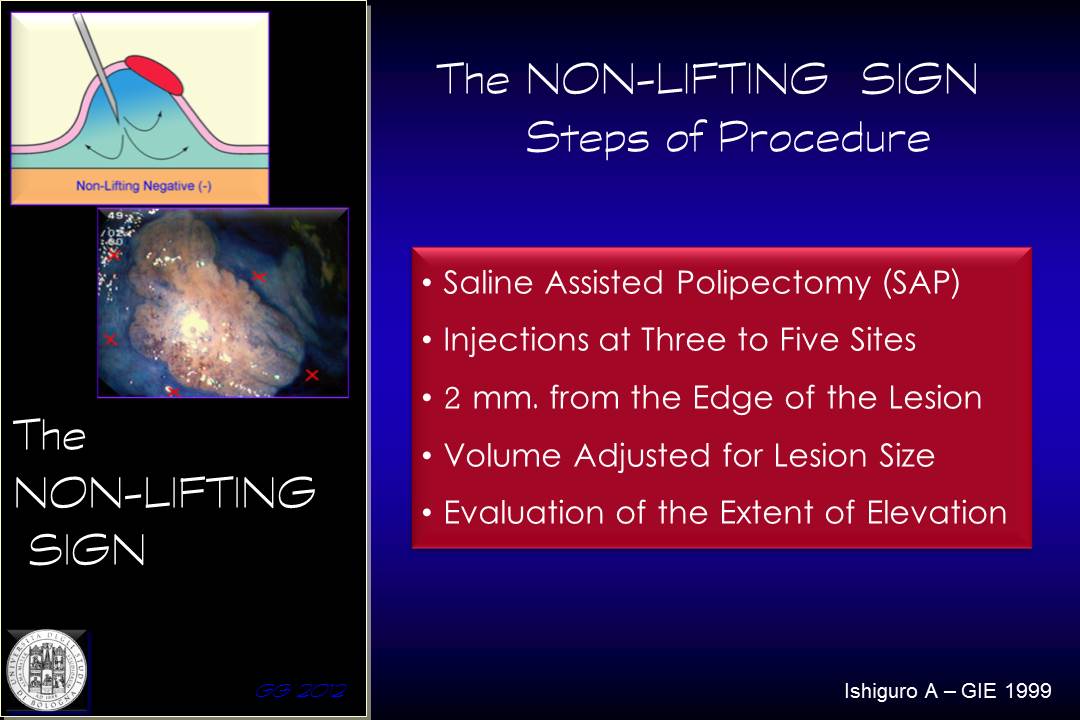
Submucosal fluid infiltration is performed at 2 mm from the margins around the lesion, in 3 to 5 different points according to the size of the lesion, and then the effect of lifting is observed.
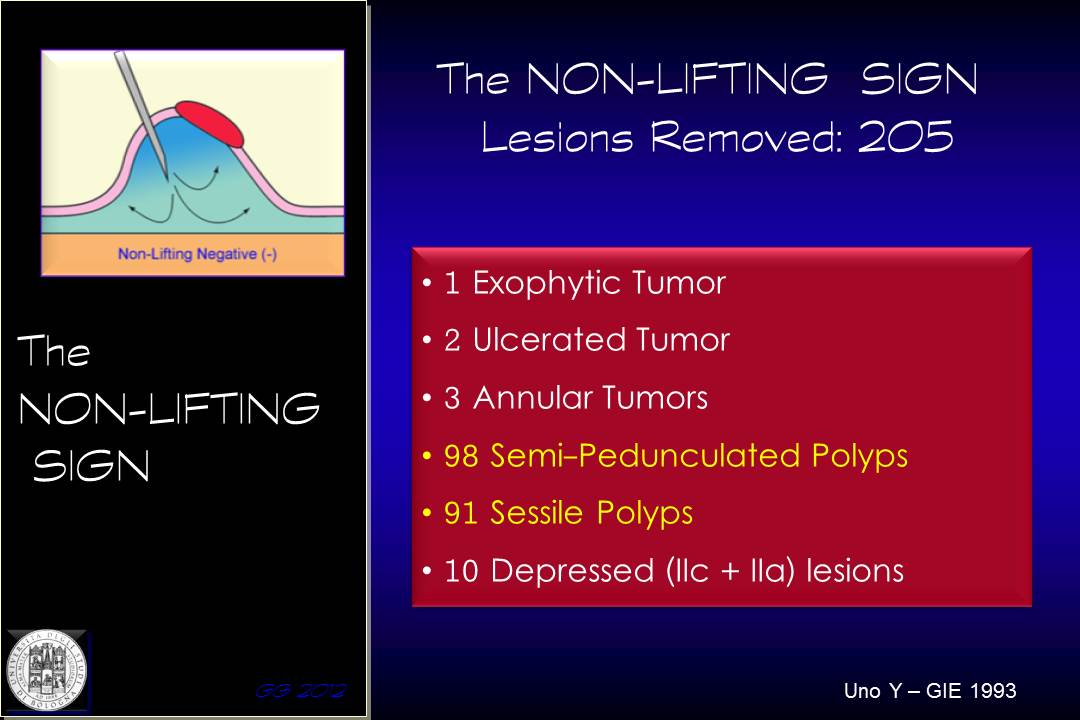
In the original study by Uno, most lesions evaluate dwere sessile or pedunculated polyps ....
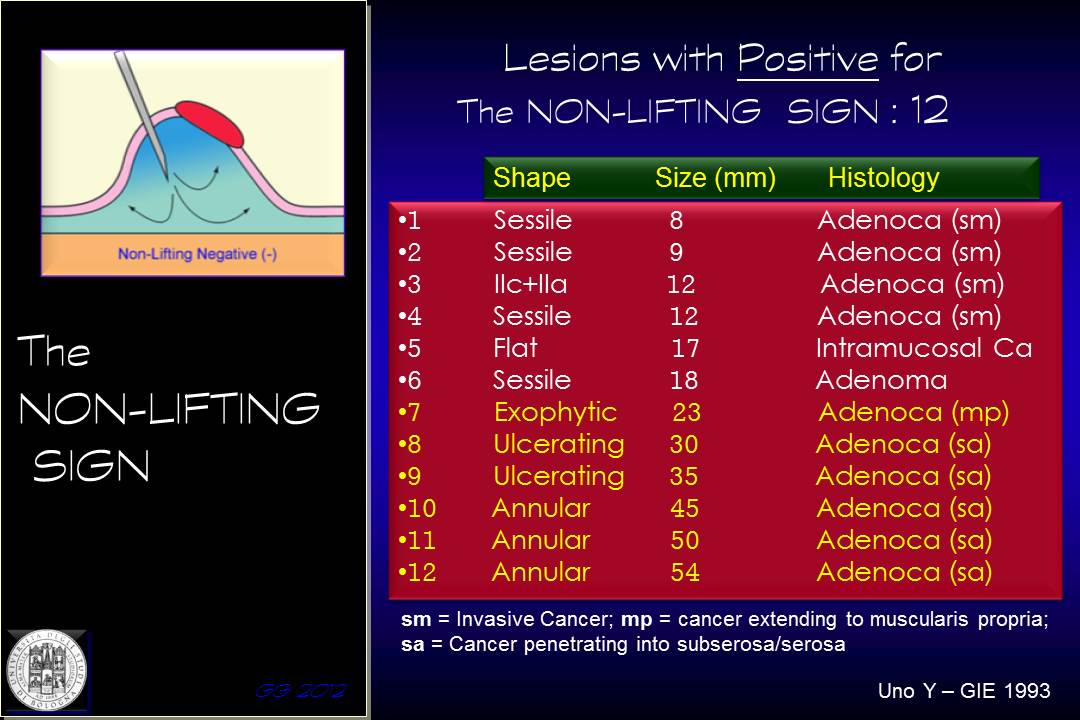
Of the 12 lesions with positive NLS, six were very advanced lesion, while the remaining were lesions within the 20 mm of diameter
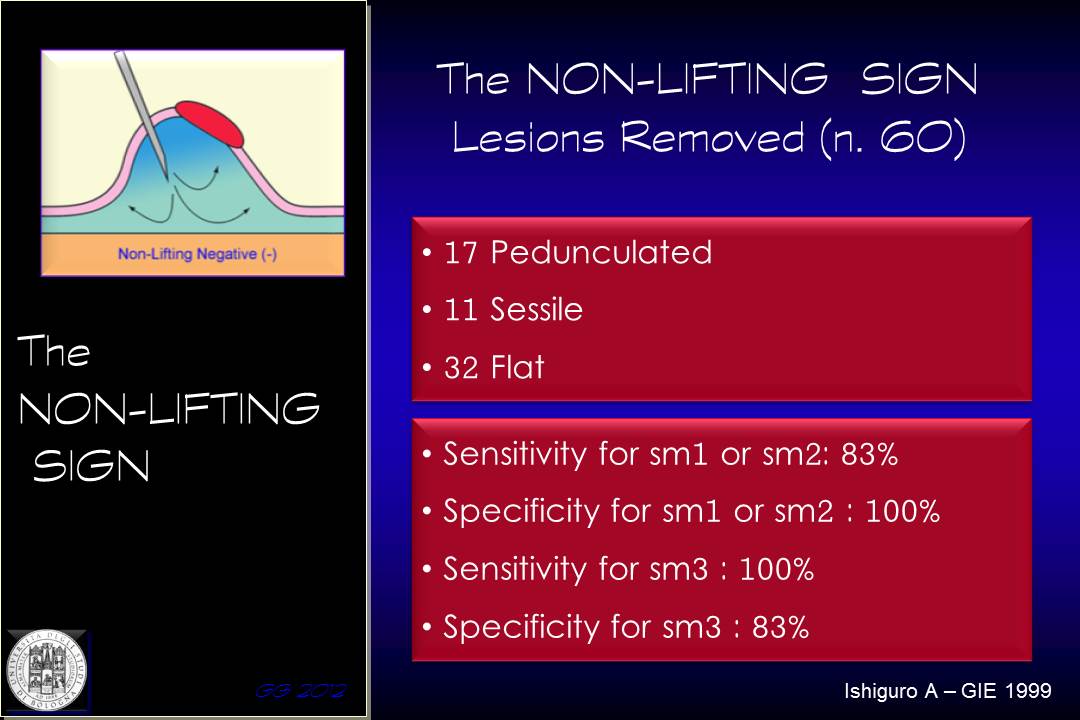
A subsequent report by Ishiguro in 1999, analysed 60 lesions, half of which were non-polypoid in shape. The NLS showed a sensitivity of 83% for less invasive lesions (sm1 and sm2), with 100% specificity, while a sensitivity and specificity of 83% in the assessment of more invasive lesions (sm3)
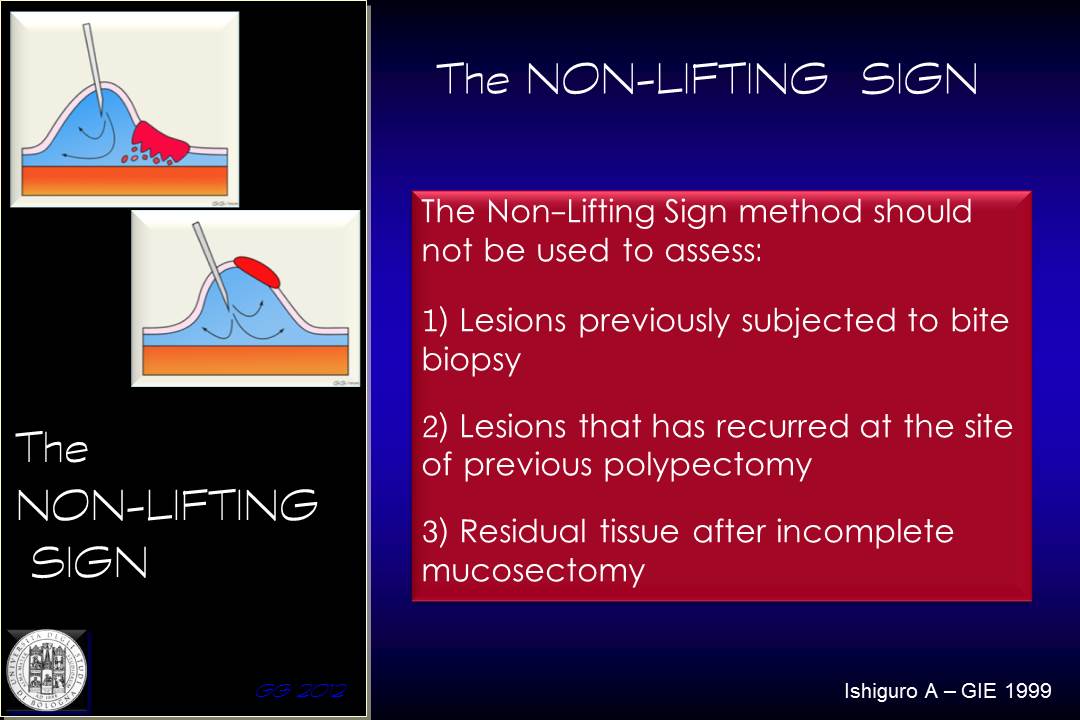
The paper from Ishiguro also demonstrated that the NLS is not reliable in case of previous biopsy, or for residual or recurrent adenomatous lesions following a prior endoscopic resection
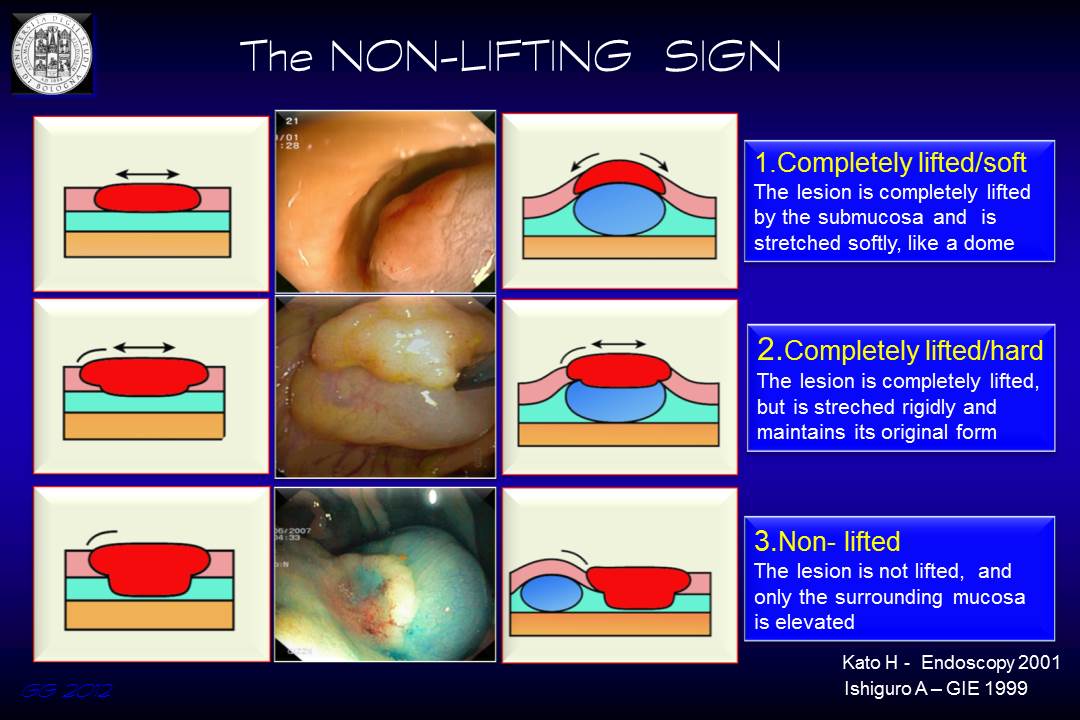
Three different scenarios can be encountered:
1) Complete response to submucosal fluid injection: the shape of the lesion adapts to the curvature of the submucosal cushion
2) Complete response to submucosal fluid injection, but the lesion keeps its initial original shape
3) Partial or no lifting of the lesion that remains in a lower plane compared to the surrounding mucosa.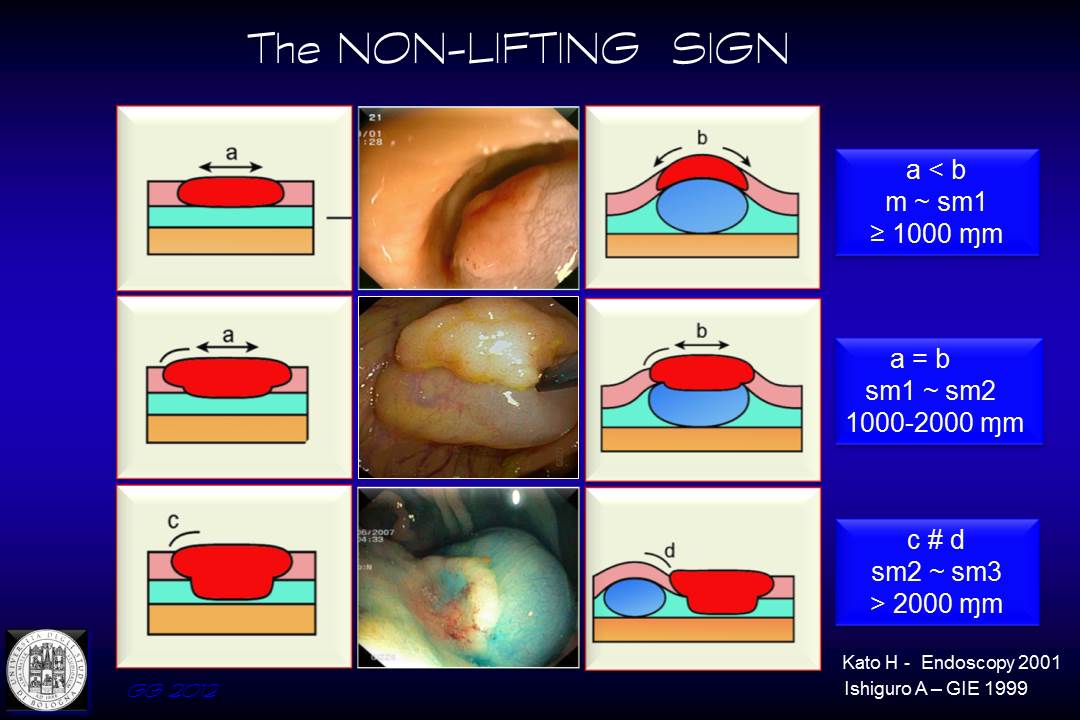
1) in the first case, the diameter of the injected lesion is larger than the initial lesion and submucosal invasion, if present doeas not crosses the superficial submucosa (sm1)
2) in the second case, the injected lesion does not modify its diameter, the submucosal invasion is comprised between sm1 and sm2
3) in the last case, with partial or no lifting, the infiltration of the submucosa is likely to be sm3
In this video the a negative NLS can be seen. The submucosal fluid injection not only confirms the presence of a superficial lesions, a serrated polyp, but also enhances the surface pattern facilitating its interpretation
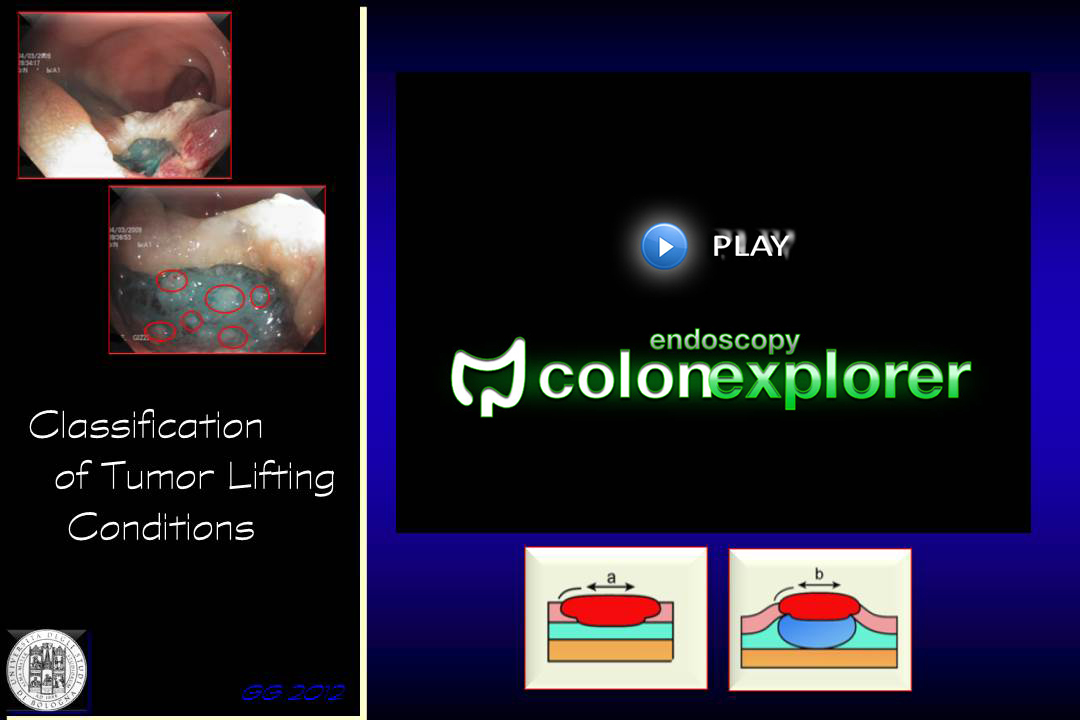
In this second video the NLS was not useful: the lesion can be lifted, despite a very suspicious macroscopic appearance, is then resected, but the persistence of “submucosal infiltration nodules” at the base of resection are appreciated. The endoscopist should bear in his/her mind the possibility that also a lesion unfit for endoscopic resection can be eventually lifted “forcing” the injection…
Also in this case, forcing the submucosal injection of a depressed lesion an apparently sufficient lifting is achieved. Nonetheless, we can appreciate that residual neoplasia is still present at the resection margin and also the dissection procedure is unfruitful and incomplete
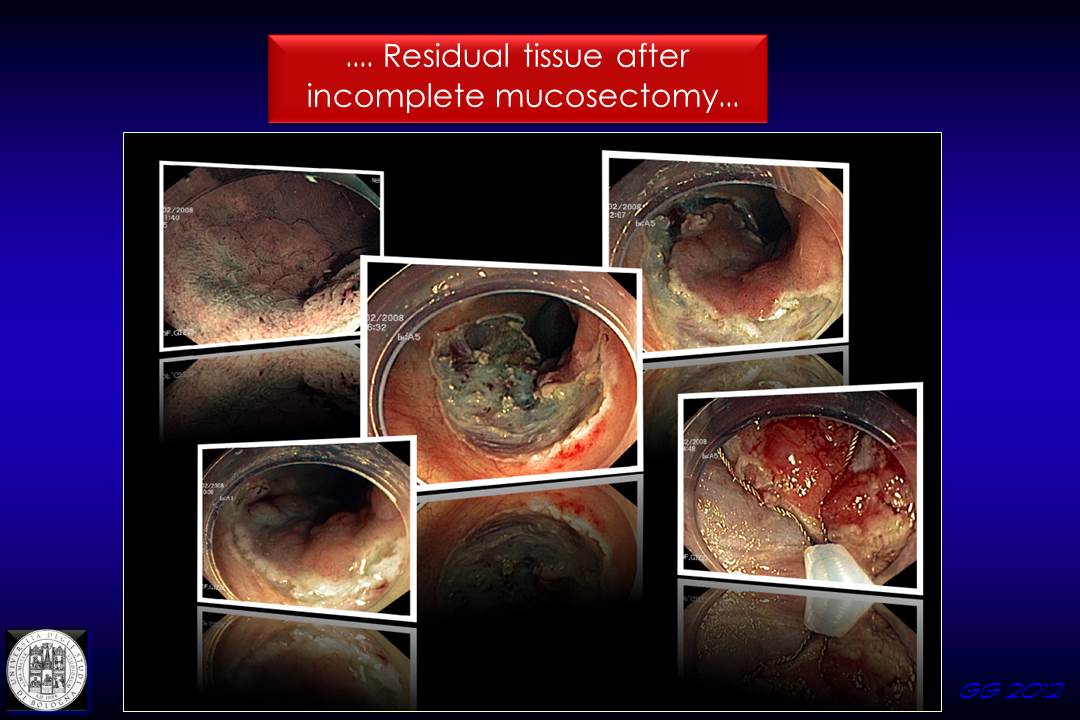
This is the case of a residual adenomatous lesion following incomplete mucosectomy. The no-lifting sign was falsely positive, and the lesion could be completely excised with diathermic snare after partial dissection with the hook-knife on the margin of the scar.
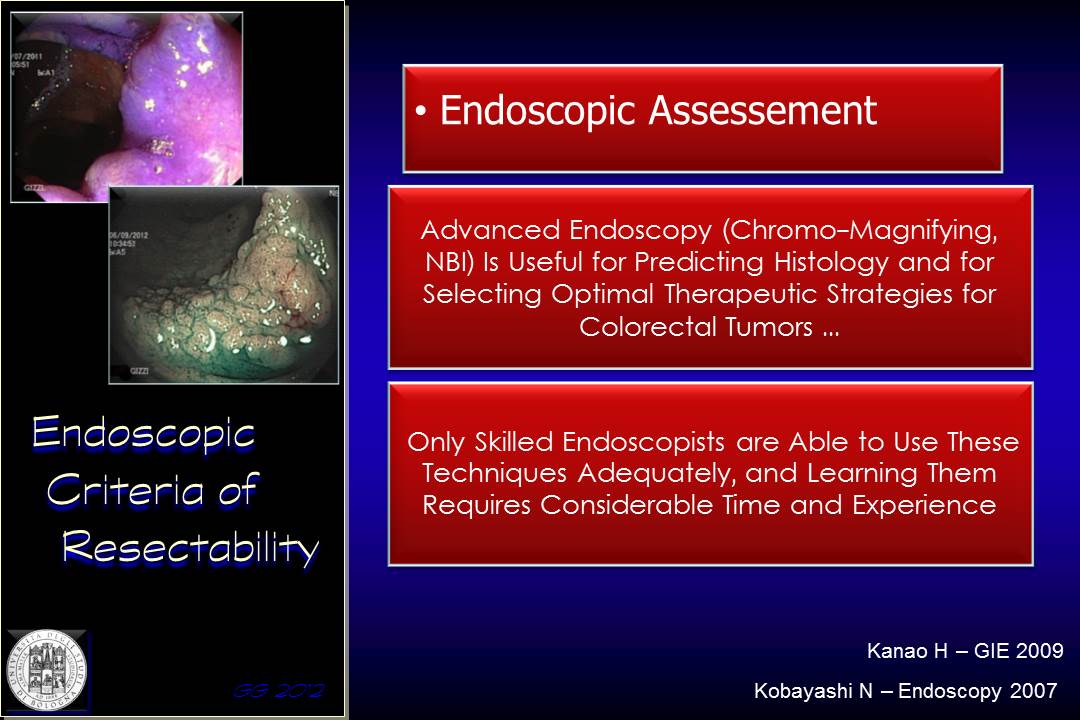
How can the endoscopic staging improve the results of the NLS? Are there situation where endoscopic assessment is superior to the NLS? Many studies have shown that the application of magnification chromo-endoscopy or NBI may accurately predict the histology of a neoplastic colorectal lesion. Such ancillary techniques are in the domain of the expert endoscopist, fully trained in the use of these enhanced imaging techniques and ready to apply advanced resection procedures
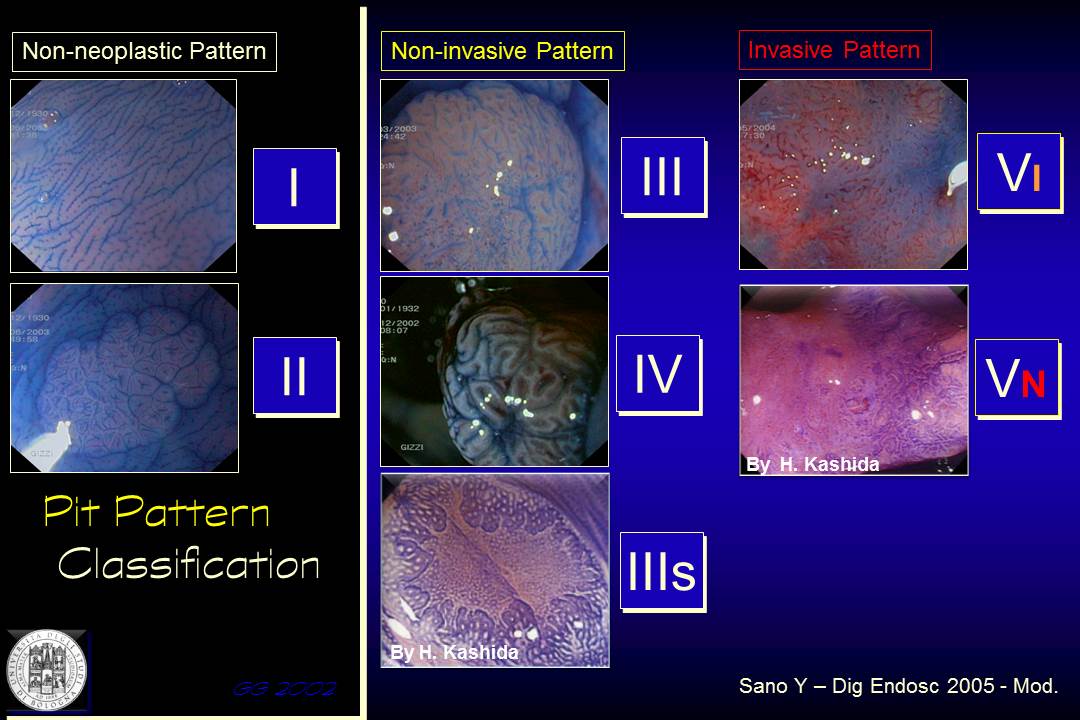
The lesion can be endoscopically categorised into non neoplastic, nepolastic non-invasive and neoplastic invasive
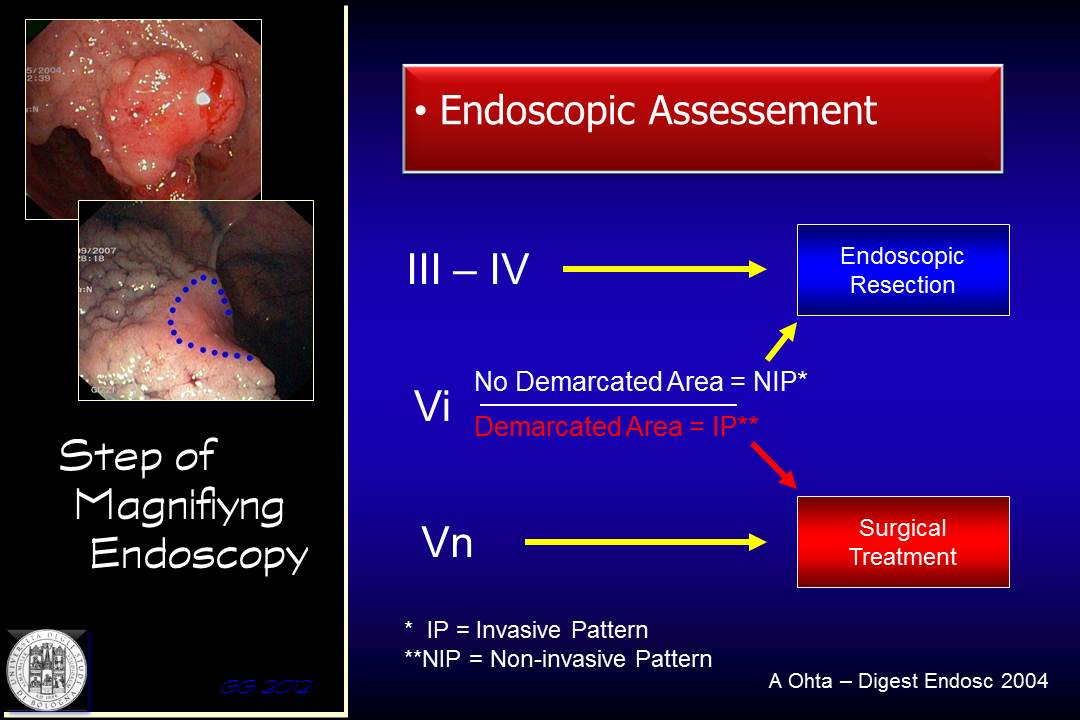
Each of these categories suggest a specific type of treatment, be it endoscopic or surgical
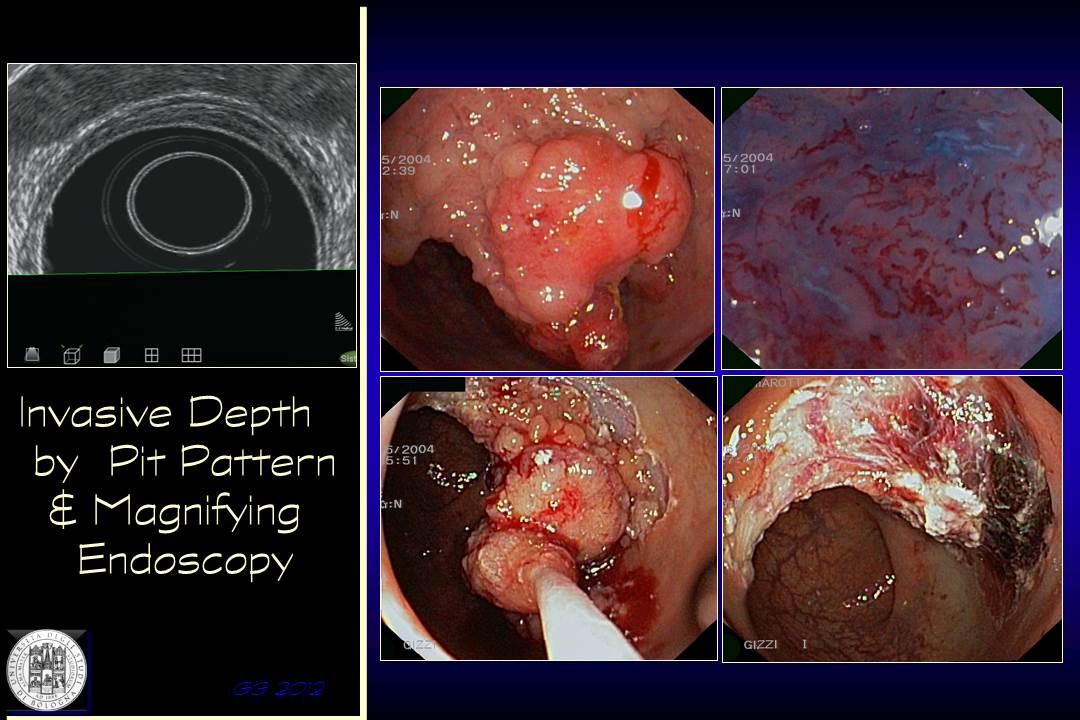
This patient was treated some years ago. The surface pattern had erroneously been categorized as low-risk for submucosal invasion and the NLS was negative. The lesion was successfully removed but histology confirmed diffuse sm2 infiltration.
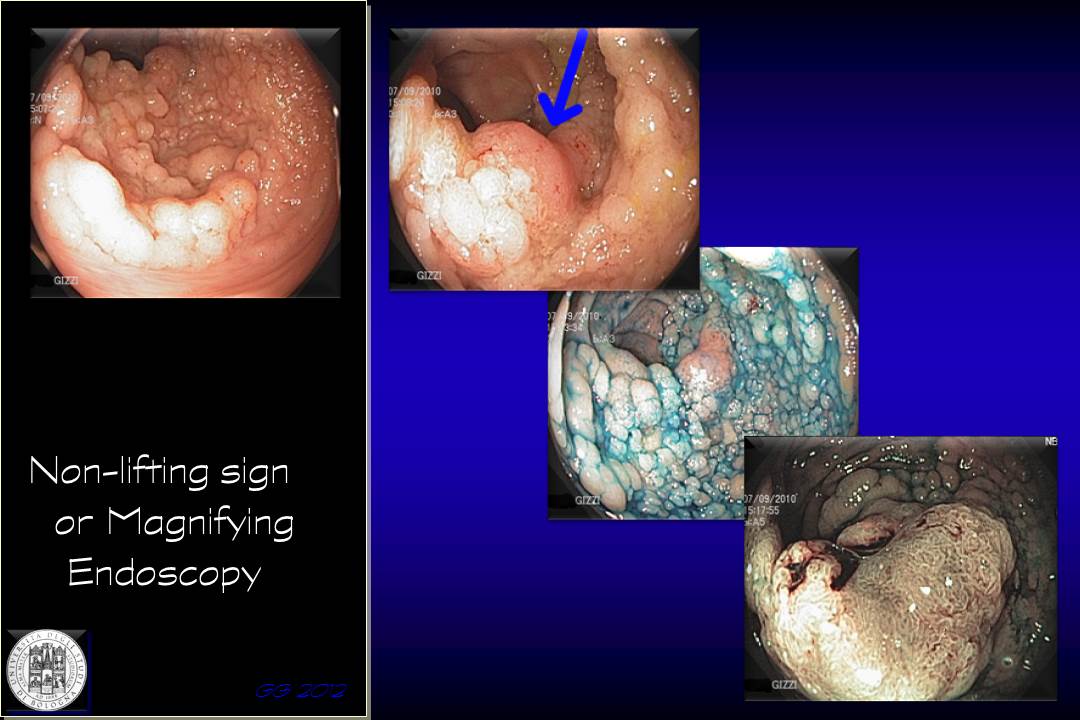
In the following case a large, granular lesion is apparently amenable to endoscopic resection
The video shows central depressed area where the pattern is still recognizable (Kudo’s Vi light), but there are consistent doubts about the utility of endoscopic removal.
The endoscopic assessment of the margins of this lesion guides to an endoscopically removable lesion, likely to have a negative NLS at the periphery of the lesion. Nonetheless, when the endoscopic assessment is completed with chromo-endoscopy, a depressed area with destructured pattern (Kudo’s Vn) can be highlighted which contraindicates the endoscopic therapeutic procedure.
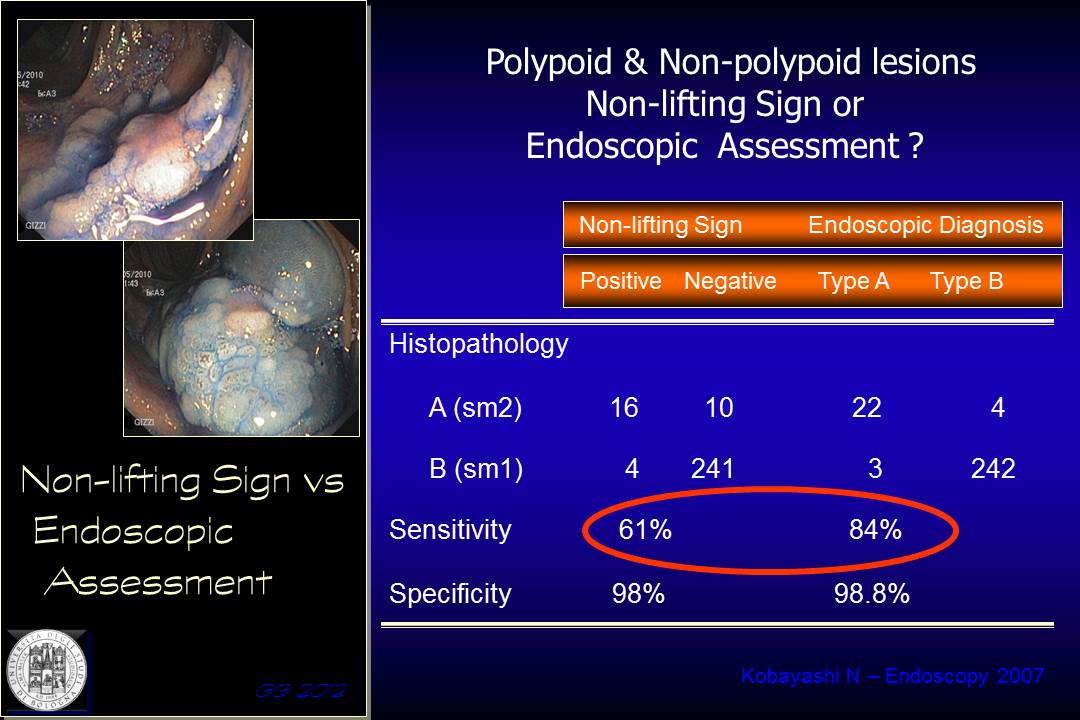
A paper by Kobayashi demonstrated that the endoscopic assessment has superior diagnostic yield compared to NLS in a consistent sample of lesions with different morphology, both polypoid and non-polypoid. The sensitivity for NLS vs. endoscopic staging was 61% and 84% respectively.
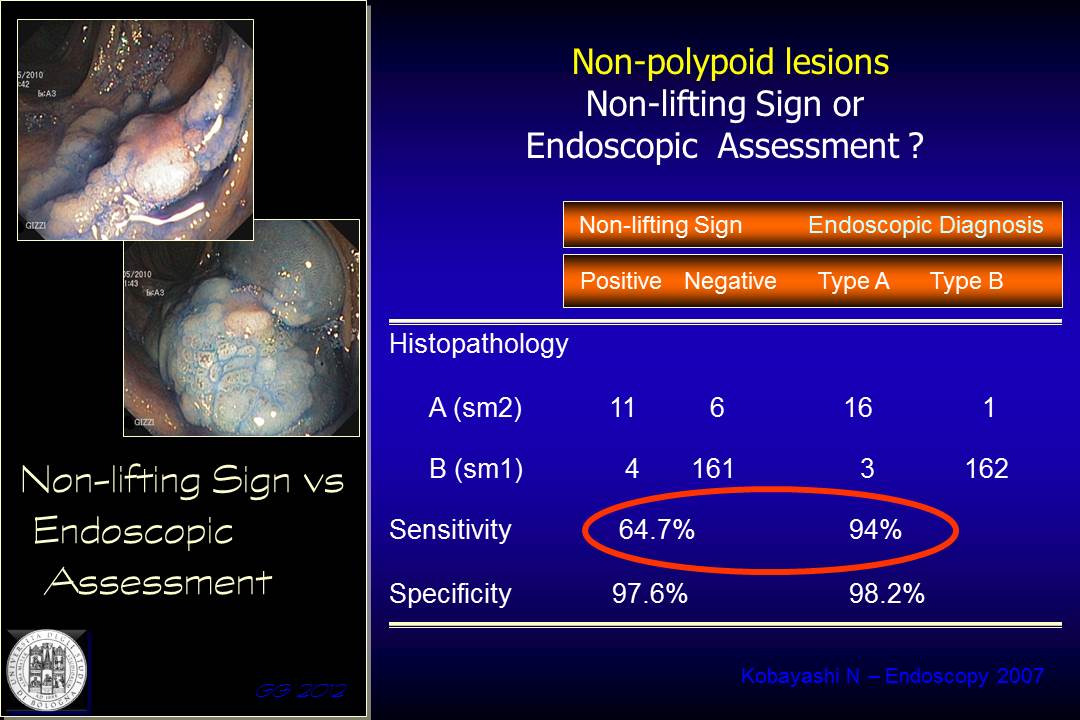
This difference is even more striking in favor of the endoscopic assessment if we take into account only the non-polypoid lesions.
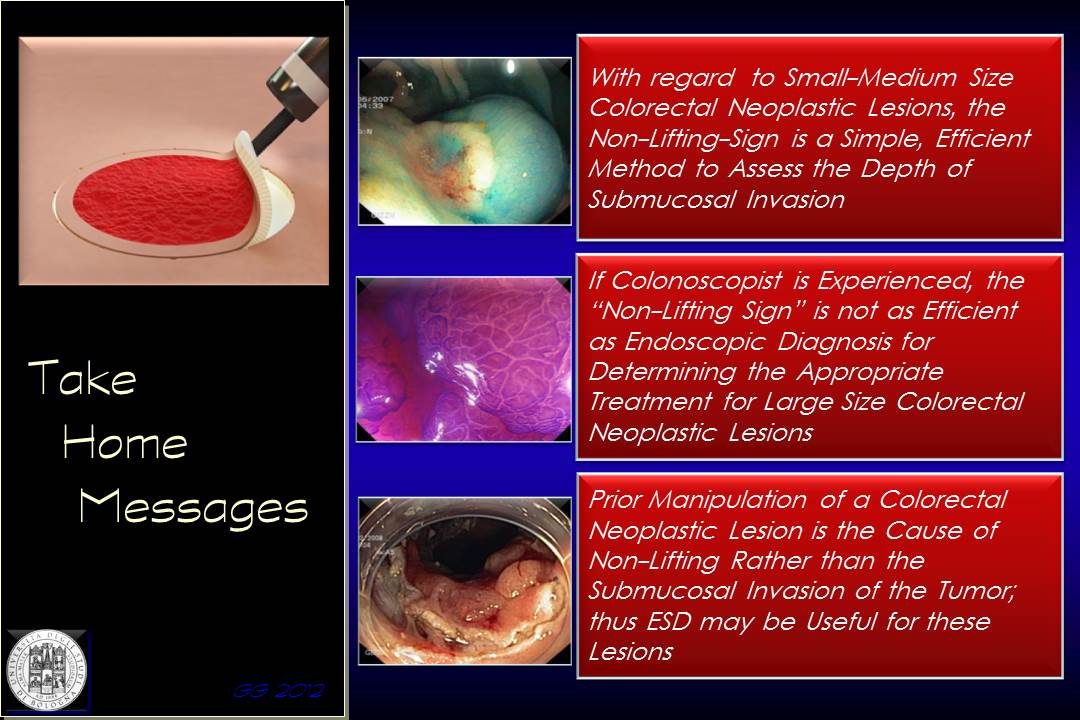
In conclusion, the NLS is a simple and effective procedure to assess endoscopic resectability of smaller lesions, a technique suitable for all endoscopists. Endoscopic assessement is more demanding, prerogative of expert endoscopist, but much more reliable in staging larger and complex lesions. Previously biopsied lesions and incomplete resections with residual or recurrent adenoma cannot be assessed with the non-lifting sign.